Understanding Functional Neurological Disorders
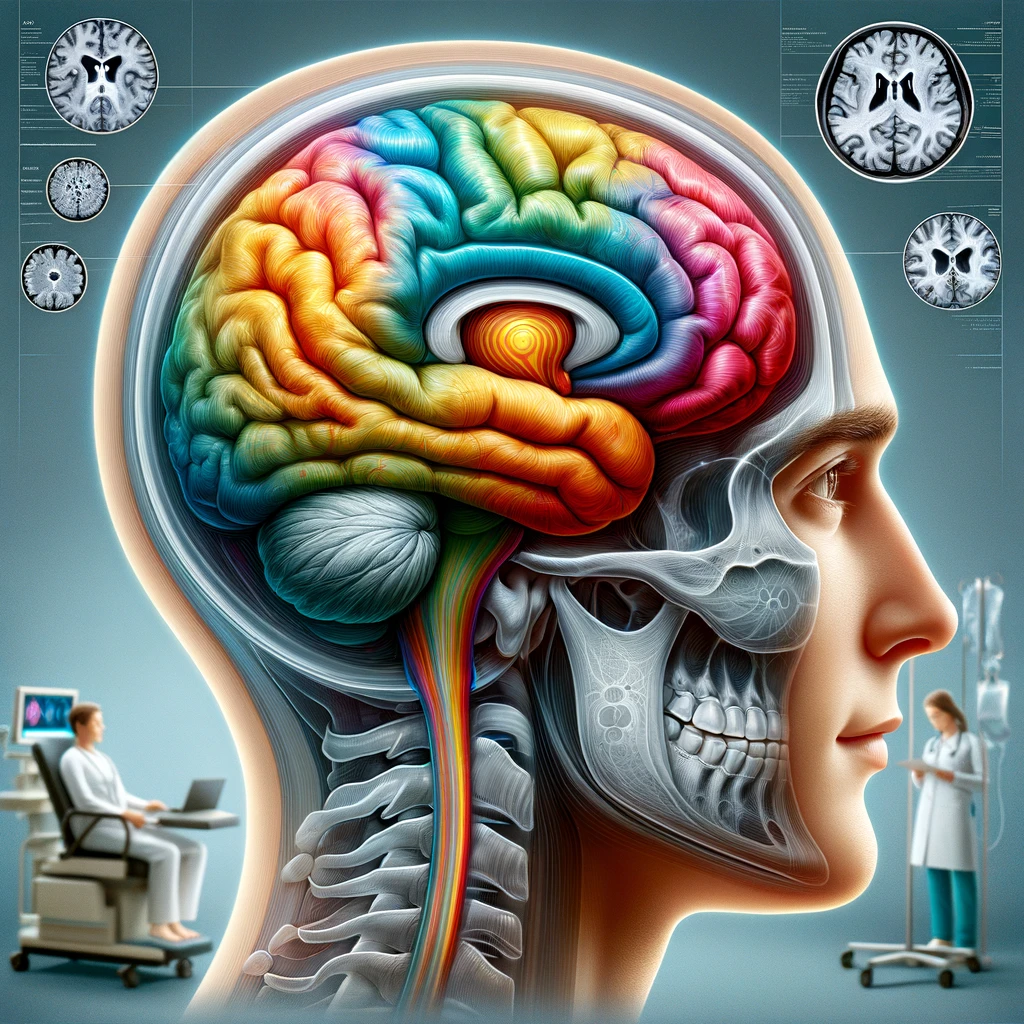
Functional Neurological Disorders (FND) represent a complex set of conditions characterized by neurological symptoms that cannot be explained by traditional medical or neurological diagnoses. These disorders originate from dysfunctions in the nervous system rather than structural damage, leading to significant challenges in both diagnosis and management. The symptoms may include tremors, weakness, paralysis, and seizures, and often fluctuate in severity and presentation. Patients may experience significant disability and distress, impacting their quality of life.
The underlying mechanisms of FND are multifaceted, involving a combination of biological, psychological, and social factors. Research suggests that these disorders may arise due to abnormal functioning of the brain networks that regulate movement and sensations, possibly influenced by psychological stressors or traumatic experiences (Edwards et al., 2020). As such, individuals with FND often possess histories of trauma, chronic pain, or anxiety disorders, linking mental health closely with the manifestation of these neurological symptoms.
Cognitive and emotional factors play a critical role in the development and persistence of FND symptoms. Cognitive processes, such as attention and anticipation of pain, can amplify physical sensations, causing a vicious cycle of fear and avoidance behaviors (Lloyd et al., 2018). It is essential for clinicians to understand these dynamics to provide appropriate care, as stigmatization or misunderstanding of the disorder can lead to unnecessary interventions, further complicating the patient’s experience.
In the clinical setting, diagnosing FND poses significant challenges. Unlike traditional neurological conditions, FND may not show abnormalities on conventional imaging or laboratory tests. Clinicians rely on careful patient histories, physical examinations, and sometimes specialized tests to differentiate FND from other neurological conditions. The use of positive clinical signs—such as inconsistent neurological findings during examinations—can aid in establishing the correct diagnosis, which is crucial because it validates the patient’s experience and opens the door to appropriate treatment approaches (Stone et al., 2010).
The misconception that FND is purely psychological can lead to inadequate treatment and potential medical legal challenges. Proper classification of FND as a legitimate neurological condition, which involves integrated care strategies addressing both neurological and psychological factors, is essential for improving outcomes and minimizing the likelihood of litigation relating to misdiagnosis or inadequate care. Implementing multidisciplinary treatment plans that encompass physical rehabilitation, psychological interventions, and patient education is vital for effective management.
Overall, gaining a comprehensive understanding of Functional Neurological Disorders provides a foundation for developing effective treatment programs. Addressing the stigma surrounding FND, fostering clinical awareness, and promoting patient-centered care can significantly enhance the approach to this often-misunderstood group of disorders, ultimately leading to better patient outcomes.
Identifying Common Obstacles
The journey toward establishing effective programs for Functional Neurological Disorders (FND) is fraught with specific obstacles that can hinder progress. A significant challenge stems from the lack of awareness and understanding surrounding FND among healthcare professionals. Many clinicians, despite their expertise in neurological disorders, may not be well-versed in the nuances of diagnosing and managing FND. This knowledge gap can lead to misdiagnosis, inappropriate referrals, and ineffective treatment strategies, which not only prolong the suffering of patients but also increase healthcare costs due to unnecessary investigations and interventions.
In addition to educational shortcomings, stigma remains a critical barrier in the management of FND. Patients often encounter skepticism from both healthcare providers and society at large, which can exacerbate their condition. This stigma can lead to feelings of isolation and frustration, as patients may perceive that their symptoms are not taken seriously. Furthermore, the association of FND with psychological factors can result in patients being dismissed or labeled inaccurately as malingerers. This perception can complicate the therapeutic relationship and discourage patients from seeking or adhering to treatment.
Another obstacle identified in developing effective FND programs is the fragmentation of care. Patients typically require a multidisciplinary approach that incorporates neurologists, psychologists, physical therapists, and occupational therapists, among others. However, in many healthcare settings, these specialists operate in silos, leading to disjointed care and communication breakdowns. Such fragmentation can prevent the timely sharing of knowledge and therapeutic strategies essential for comprehensive treatment, ultimately hindering the recovery process.
Access to care is also a significant barrier influencing patient outcomes. In many regions, facilities specializing in FND are limited, necessitating long-distance travel for affected individuals. This logistical challenge can lead to missed appointments and inconsistent follow-up care. Moreover, financial constraints related to healthcare access can exacerbate this issue, making it difficult for patients to pursue comprehensive treatment programs and limiting their engagement with necessary resources.
Additionally, the dynamic nature of FND symptoms presents another layer of difficulty. Patients may experience fluctuations in their symptoms, complicating treatment adherence and response to interventions. This variability can result in frustration on both the part of patients and healthcare providers, as it may be difficult to establish stable treatment protocols.
Clinicians should also be aware of the medicolegal implications associated with the management of FND. Given the complexity of these disorders and the potential for misdiagnosis, clinicians may face litigation if patients feel inadequately treated or misunderstood. Clear documentation of clinical findings, treatment rationales, and ongoing patient communication become crucial in mitigating risks associated with legal challenges. Establishing clear treatment protocols and integrated communication within multidisciplinary teams can help reduce discrepancies in care that may lead to legal disputes.
Lastly, insufficient funding and resources for research and training pose a substantial obstacle to the development of FND programs. Many healthcare systems prioritize more prevalent neurological disorders, leaving FND underfunded and under-researched. This lack of investment stifles innovation in treatment strategies and hinders program development that could address FND’s unique challenges. Consequently, advocacy for increased recognition and resources dedicated to FND is imperative to create sustainable and effective treatment frameworks.
Addressing these common obstacles is essential for advancing the development of FND programs. An awareness of these challenges enables clinicians and healthcare systems to proactively devise solutions, improving care delivery and ultimately enhancing patient outcomes.
Strategies for Program Development
Developing an effective program for Functional Neurological Disorders (FND) necessitates a multifaceted approach that addresses the intricate nature of these conditions and the surrounding healthcare environment. One of the primary strategies is to foster a culture of awareness and education among healthcare professionals. This can be accomplished through targeted training workshops, seminars, and continuing medical education focused specifically on FND. Incorporating case studies and patient testimonials may enhance understanding and empathy, enabling clinicians to recognize the complexities and realities faced by individuals with these disorders (Edwards et al., 2020).
In addition to professional education, patient education programs are crucial. Providing resources that explain FND in accessible language helps patients and their families better understand the condition, acknowledges their experiences, and empowers them to take an active role in their treatment (Lloyd et al., 2018). This can include printed materials, videos, and support groups where experiences and management strategies can be shared. Joint educational initiatives that involve both clinicians and patients can further strengthen the therapeutic alliance, fostering a more supportive treatment environment.
Creating a multidisciplinary care team is another cornerstone strategy for program development. An integrated approach that includes neurologists, psychologists, physical therapists, and occupational therapists ensures that all aspects of a patient’s well-being are addressed. Regular interdisciplinary meetings facilitate communication, enabling healthcare providers to share insights, updates, and treatment plans. This cohesive strategy not only streamlines care but also helps in aligning treatment objectives, thus improving patient adherence and outcomes.
To address the issue of care fragmentation, utilizing a case management system can be advantageous. Designating case managers or care coordinators who oversee patient journeys from initial diagnosis through follow-up can help mitigate the risk of disjointed services. These coordinators can provide consistent points of contact for patients, ensuring they receive timely access to necessary consultations and therapies. This continuity of care can be particularly important for those experiencing fluctuating symptoms, as it can help maintain treatment engagement even during challenging periods.
Moreover, the integration of telemedicine into FND programs can enhance accessibility for patients who may have difficulty attending in-person appointments. Telehealth services can provide virtual consultations, follow-ups, and educational sessions, reducing barriers related to travel, time, and cost. Utilizing remote monitoring tools that allow patients to track their symptoms and progress can facilitate ongoing communication with healthcare providers, leading to more responsive and adaptable treatment plans.
Incorporating personalized treatment plans is essential for addressing the variability associated with FND symptoms. Each patient’s experience with FND is unique, and treatments should be tailored to their specific needs and circumstances. Regularly updating treatment protocols based on symptom fluctuations and patient feedback will enhance individualization and responsiveness. Employing a phased approach, where treatment intensifies or adapts according to the patient’s evolving needs, can be particularly effective.
Funding and research advocacy is critical in advancing FND programs. By seeking partnerships with research institutions, healthcare organizations can support studies that explore the underlying mechanisms of FND and evaluate the effectiveness of various treatment modalities. Grant applications and collaborative projects can also attract funding that facilitates the development and implementation of innovative treatment programs. Furthermore, advocating for increased awareness and prioritization of FND within medical and policy circles can garner the necessary support for long-term sustainability.
Establishing clear metrics for evaluating treatment effectiveness and program impact is vital. Utilizing standardized assessments for symptom severity, functional outcomes, and quality of life can provide objective measures of progress. Regular analysis of these metrics will allow for continuous improvement of the program, identifying successful strategies while recognizing aspects needing adjustment. This commitment to ongoing evaluation not only enhances patient care but also bolsters credibility in medical and legal contexts, reducing risks associated with mismanagement (Stone et al., 2010).
Engaging patients in the design and refinement of FND programs can offer valuable insights and foster a sense of ownership over their treatment journey. Patient advisory boards or feedback mechanisms can be employed to gather perspectives that guide program development, ensuring that services are patient-centered and responsive to real needs.
All these strategies converge into a holistic approach aimed at providing comprehensive, empathetic care to individuals with Functional Neurological Disorders. Improving education, fostering interdisciplinary collaboration, enhancing accessibility, and personalizing treatment are pivotal in transforming FND care, ultimately leading to better patient outcomes and satisfaction.
Evaluating Program Effectiveness
Evaluating the effectiveness of programs designed for Functional Neurological Disorders (FND) is essential for ensuring that interventions meet patient needs and improve outcomes. A systematic approach to evaluation involves collecting data on clinical outcomes, patient satisfaction, and the overall impact of the program on healthcare utilization. By employing various evaluation methods, healthcare providers can gather insightful information that informs ongoing practice and program development.
One of the primary measures of evaluating program effectiveness is the use of standardized clinical assessments. Tools such as the Functional Neurological Disorder Severity Scale (FNDSS) or the Hospital Anxiety and Depression Scale (HADS) allow clinicians to quantitatively assess the severity of symptoms and the psychological status of patients before, during, and after treatment. These instruments can help track improvements in motor function, psychological well-being, and quality of life, providing a clear picture of treatment efficacy over time. Regular assessments help in identifying trends that can inform clinical decision-making and adjustments to treatment plans as necessary.
Patient-reported outcomes (PROs) are also critical in evaluating the success of FND programs. Surveys and questionnaires that solicit patient feedback about their symptoms, perceived recovery, and overall satisfaction with care can reveal valuable insights into how treatments impact their daily lives. Engaging patients in this evaluative process fosters a sense of collaboration and ownership over their care while providing healthcare providers with qualitative data that may not emerge through clinical metrics alone. The incorporation of tools like the Patient-Reported Outcomes Measurement Information System (PROMIS) can further refine the analysis of patient experiences and enable a deeper understanding of treatment effects.
Longitudinal studies offer another robust method for evaluating program effectiveness. By following cohorts of patients over extended periods, researchers can assess the durability of treatment effects and the prevalence of relapses or symptom fluctuations. This approach allows for a comprehensive understanding of how FND interventions perform over time, which is particularly vital given the fluctuating nature of these disorders. Such studies can illuminate factors contributing to long-term success or challenges, guiding improvements in treatment strategies.
In addition to clinical outcomes, the functional impact of FND treatment can be measured through assessments of patients’ abilities to return to daily activities, work, and social engagements. Evaluating changes in functional status before and after interventions can provide a practical perspective on the benefits of the program, directly linking clinical improvements to patients’ quality of life. Functional recovery can be quantified using measures such as the Brief Resilience Scale (BRS), which assesses the ability to bounce back from stressors, providing insights into the psychological resilience following treatment.
Healthcare utilization metrics can also serve as indicators of program effectiveness. Monitoring rates of hospitalizations, emergency department visits, and the need for additional interventions provides a contextual backdrop to evaluate whether the program effectively reduces the burden of FND on the healthcare system. A decrease in these metrics post-intervention can indicate that the program is yielding substantial benefits not just for patients, but also for healthcare resources, highlighting its value in a broader context.
In the realm of medicolegal relevance, systematic evaluation of FND programs can further enhance clinician risk management practices. Clearly documented evidence of treatment efficacy—backed by data from assessments and patient feedback—can significantly bolster a clinician’s defense against potential litigation. Informed consent, built through transparent communication regarding treatment goals and expected outcomes, can be reinforced by robust evaluation data, significantly increasing the credibility of care provided.
Moreover, the establishment of feedback loops within program evaluations encourages continuous improvement. Regularly scheduled reviews that incorporate the examination of collected data, alongside feedback from both patients and clinical staff, can facilitate dynamic adaptations to the program. This ongoing development reflects a commitment to excellence in care and aligns with best practices in healthcare, encouraging a culture of quality enhancement rather than stagnation.
Lastly, sharing the results of program evaluations publicly or within professional networks contributes to collective learning in the field of FND. Disseminating findings through peer-reviewed journals or conferences allows the broader medical community to benefit from successful strategies and pitfalls encountered during implementation. This transparency not only advances the understanding of FND but also fosters collaboration and innovation across various healthcare systems and specialties.
In summary, a multifaceted evaluation strategy that incorporates clinical, functional, and patient-reported outcomes, alongside healthcare utilization metrics, is integral to understanding the effectiveness of FND programs. This comprehensive evaluation framework not only improves patient care but also strengthens the clinical practice landscape, enhancing the overall treatment of Functional Neurological Disorders.