Patient-Centered Approach
A patient-centered approach emphasizes the importance of understanding the individual experience of those with functional neurological disorders (FND). This model prioritizes the needs and preferences of patients, recognizing that each person’s presentation of symptoms may be unique and influenced by a multitude of factors including psychological, social, and biological components. In practice, this means that healthcare providers must engage in active listening, validating the patient’s concerns, and fostering an environment in which patients feel respected and empowered to participate in their care.
One key aspect of this approach is the development of strong therapeutic relationships between patients and healthcare providers. Establishing trust allows for better communication, enabling patients to openly discuss their symptoms and any underlying issues without fear of stigma or misunderstanding. Patients often report feeling more satisfied with their care when they are involved in decision-making processes about their treatment options, which can lead to better adherence to therapeutic strategies and improved outcomes.
Importantly, a patient-centered approach takes into account the holistic well-being of individuals, addressing not only their physical symptoms but also their emotional and psychological needs. This might involve integrating mental health assessments and support into the management of FND, recognizing that psychological factors can play a significant role in symptom manifestation. Therapies such as cognitive behavioral therapy (CBT) can be particularly beneficial, helping patients develop coping strategies and address maladaptive thoughts that may exacerbate their condition.
Furthermore, this approach is clinically relevant as it supports personalized treatment plans tailored to the specific circumstances and preferences of the patient. This may include coordinating care among different health professionals, such as neurologists, psychologists, physiotherapists, and occupational therapists, to provide a comprehensive care strategy that aligns with the patient’s goals.
From a medicolegal standpoint, implementing a patient-centered model can also have implications for liability and informed consent. Clear communication and mutual understanding of treatment plans can help mitigate potential disputes, ensuring that patients are aware of the nature of their condition and involved in the decision-making regarding their care. Fostering an inclusive discussion can aid in managing expectations and reinforce the importance of patient education, which is vital in the context of EFD where there may be misconceptions about the nature of the disorder.
Neuropsychiatric Integration
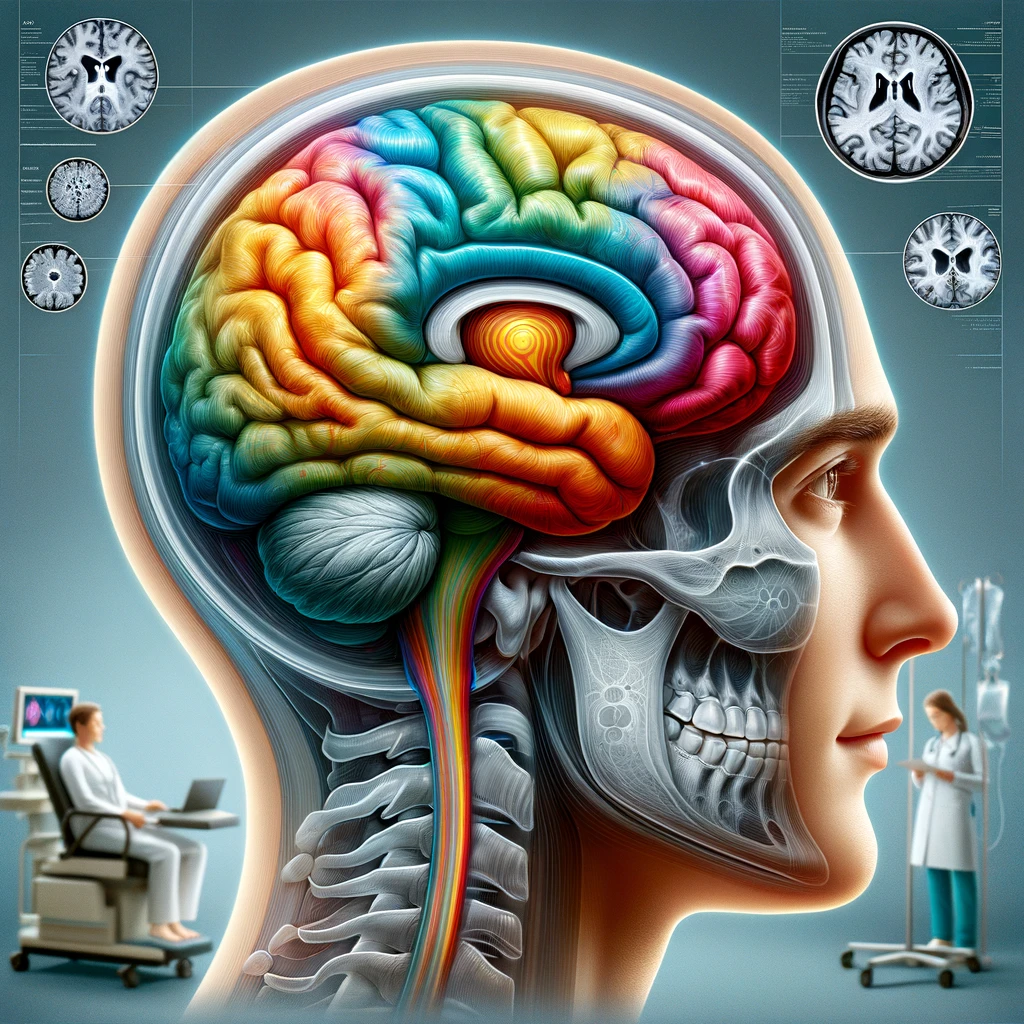
Neuropsychiatric integration is a vital element of managing functional neurological disorders (FND), recognizing the intertwined relationship between neurological and psychiatric aspects of these conditions. Patients often experience symptoms that cannot be easily categorized into purely neurological or psychological domains. Thus, it is essential that healthcare practitioners adopt an interdisciplinary approach that incorporates both neurological and psychiatric perspectives for the comprehensive management of FND.
Clinically, this integration fosters a deeper exploration of the biochemical, structural, and functional aspects of the brain that can influence behavioral patterns. Studies illustrate that patients with FND may exhibit atypical patterns in neuroimaging, highlighting the relevance of brain functionality beyond standard neurological symptoms. Integrating psychiatric evaluations can illuminate underlying psychological stresses or trauma that may be contributing to a patient’s condition. Psychotrauma, for instance, is frequently observed in patients experiencing dissociative symptoms within FND, suggesting a potential pathway toward symptom manifestation that warrants exploration through a psychiatric lens.
Furthermore, neuropsychiatric integration encourages healthcare providers to utilize a variety of psychological interventions aligned with neurological treatment. This might include the referral to psychotherapists specializing in trauma-focused therapy or cognitive behavioral therapy, depending on the individual’s presentation. Research strongly supports the efficacy of combined therapeutic strategies; for example, patients benefiting from both medication for associated anxiety or depression and psychotherapy often demonstrate improved overall outcomes and reduced symptom severity.
Aside from treatment implications, neuropsychiatric integration has significant implications in the realm of communication between healthcare providers. Neurologists need to collaborate actively with psychiatrists and psychologists, ensuring continuity of care and a clear understanding of each profession’s insights into the patient’s condition. Regular interdisciplinary meetings can optimize patient management plans and clarify how each therapy contributes to the overall treatment objectives.
Moreover, the integration of neuropsychiatry carries medicolegal importance, particularly concerning patient consent and understanding of their disorder. When patients receive clear communication concerning the multifaceted nature of their condition, it can reduce stigma and enhance their willingness to engage in treatments that they may have previously viewed with skepticism. Establishing this understanding is key to managing potential legal challenges stemming from misinterpretation of symptoms. Empowering patients with knowledge about the neuropsychiatric basis of FND can also aid in bolstering resilience against potential accusations of ‘faking’ symptoms, thus supporting both legal and ethical practice in care delivery.
Ultimately, the integration of neuropsychiatry into the framework of FND management not only promotes holistic care but also strengthens the overall therapeutic alliance between patients and providers. By recognizing and addressing the complex interactions between neurological and psychological components, a more effective and compassionate path toward healing can be established.
Assessment and Diagnosis
Accurate assessment and diagnosis of functional neurological disorders (FND) are crucial, as they lay the groundwork for effective management and treatment. Unlike traditional neurological conditions, FND often presents with a combination of unexplained physical symptoms that do not align with recognized neurological conditions. This ambiguity can complicate the diagnostic process, necessitating a thorough and nuanced evaluation strategy.
The diagnostic process for FND typically begins with a comprehensive clinical history and physical examination. Healthcare providers must engage in active listening to capture the patient’s narrative fully, including the onset, progression, and context of symptoms. Symptoms such as non-epileptic seizures, paralysis, or gait abnormalities may occur without identifiable organic pathology. It is essential that clinicians approach these symptoms without preconceived notions or bias, recognizing the legitimacy of the patient’s experience, even when diagnostic tests yield normal results.
Diagnostic criteria for FND have been established, notably through the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) and the ICC (International Classification of Diseases). These frameworks emphasize the importance of identifying motor or sensory symptoms that are inconsistent with medical or neurological conditions, thus allowing for the classification of the disorder. A multidisciplinary approach often yields the best results, wherein neurologists, psychiatrists, and psychologists collaborate to assess the patient from various angles, ensuring that both neurological and psychological factors are considered.
Incorporating additional diagnostic tools can enhance the assessment process. For example, neuroimaging studies such as MRI or CT scans can help rule out structural brain abnormalities, while tools like EEG can differentiate between seizure types. However, it is critical to interpret these examinations in the context of the clinical picture, as the goal is not merely to identify neurological anomalies but to understand how these findings correlate with the overall symptomatology.
Clinical questionnaires may also play a role in assessment. Instruments that capture the severity and impact of symptoms, along with psychological questionnaires assessing anxiety, depression, and trauma history, provide valuable insights into the functional limitations and emotional landscape of the patient. These assessments can aid in identifying comorbid conditions, which are frequently present among those with FND—such as mood disorders, PTSD, or other anxiety disorders.
With regard to clinical practice, forming a diagnosis of FND inappropriately can breed significant skepticism in patients, complicating their well-being and treatment adherence. Thus, practitioners must communicate findings clearly, helping to demystify the diagnosis. It is also essential to educate patients regarding the nature of FND, emphasizing that the absence of organic findings does not equate to a lack of validity of their symptoms.
From a medicolegal perspective, thorough documentation of the assessment process is imperative. This includes the rationale for diagnosis, the assessment tools utilized, and any patient statements regarding their experiences. Such documentation is essential for establishing a clear clinical record and can shield providers from potential litigation stemming from misdiagnosis or misunderstandings about the legitimacy of a patient’s symptoms. Furthermore, enhancing the patient’s understanding of their diagnosis can mitigate feelings of frustration or doubt, ultimately fostering a more collaborative relationship going forward.
A comprehensive assessment for FND involves a meticulous balance of clinical evaluation, psychological insight, and clear communication, all of which are vital in reaching an accurate diagnosis and formulating an effective treatment plan. The integration of a multi-faceted assessment strategy not only aids in developing personalized care plans but also significantly influences the therapeutic relationship and patient outcomes.
Therapeutic Strategies
Therapeutic strategies for addressing functional neurological disorders (FND) must be multifaceted, involving not just pharmacological treatments, but also psychotherapeutic approaches and the incorporation of physical rehabilitation. This diverse strategy allows for a comprehensive understanding of the disorder while addressing the individual needs of patients.
At the forefront of therapeutic interventions is the use of psychotherapeutic modalities. Cognitive Behavioral Therapy (CBT) has emerged as one of the most effective treatments for FND, helping patients to identify and modify maladaptive thought patterns that may contribute to their symptoms. Studies have demonstrated that CBT can lead to significant reductions in symptom severity and improvements in quality of life for patients with FND. Furthermore, therapies that focus on trauma, such as Eye Movement Desensitization and Reprocessing (EMDR), can be beneficial, particularly for individuals whose symptoms may be linked to past psychological trauma.
In addition to psychotherapy, physical rehabilitation plays a critical role in the management of FND. Occupational therapy and physiotherapy are integral in helping patients regain functional abilities and mobility. Tailored exercises assist in re-establishing movement patterns and improving physical function, while occupational therapy focuses on enabling patients to participate in daily activities. Education on physical symptoms, such as understanding the mechanisms behind non-epileptic seizures or functional weakness, can empower patients and reduce anxiety about their conditions, leading to more effective recovery.
From a pharmacological standpoint, the management of associated comorbid conditions—such as anxiety, depression, or other mood disorders—is vital. Medications like selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help stabilize mood and address the psychological underpinnings of FND symptoms. Coordination among healthcare providers is crucial here, ensuring any pharmacological intervention complements psychotherapeutic and rehabilitation strategies.
Another promising avenue is the utilization of multidisciplinary care teams that facilitate an integrated approach to treatment. These teams typically consist of neurologists, psychiatrists, psychologists, physiotherapists, and occupational therapists, working collaboratively to devise comprehensive management plans tailored to individual patient needs. Regular meetings among team members can help in sharing insights and progress, which is essential for adjusting treatment strategies as necessary and ensuring that all aspects of the patient’s care are aligned.
Clinically, employing diverse therapeutic strategies not only enhances patient engagement but has been linked to better treatment adherence and outcomes. As patients perceive their treatment as holistic and inclusive of their concerns, they are more likely to remain committed to their care plans. Fostering a supportive environment wherein patients feel both heard and involved in their treatment fosters trust and the potential for better recovery trajectories.
The medicolegal implications of these therapeutic strategies cannot be overstated. Comprehensive documentation of the therapeutic approach, progress, and patient feedback is essential to protect healthcare providers against potential claims of neglect or inadequate care. Ensuring that patients are well-informed about their treatment options and the rationale behind them can also reduce misunderstandings that may lead to disputes. Informed consent clarifies the nature of treatment strategies, empowering patients and fostering collaborative relationships which can serve to mitigate legal risks.
Ultimately, a holistic framework that seamlessly integrates psychological support, physical rehabilitation, and pharmacotherapy, while actively involving the patient in their own care, represents the most effective therapeutic strategy for managing functional neurological disorders. Such an approach not only aims to alleviate symptoms but also supports patients in achieving greater autonomy and improved overall quality of life.