Foreign Accent Syndrome
Foreign Accent Syndrome (FAS) is an uncommon speech disorder where individuals develop a new, seemingly foreign accent in their native language. This review explores FAS within the contexts of functional neurological disorders (FND) and mild traumatic brain injuries (mTBIs).
In FNDs, FAS is often classified as a functional speech disorder, where no definitive structural brain lesions or neurological causes are identified. Cases suggest a psychogenic or functional origin, possibly triggered by psychological stress. Studies highlight that FAS in FNDs features inconsistencies and intermittency in speech patterns, which can occur even in the presence of structural brain damage.
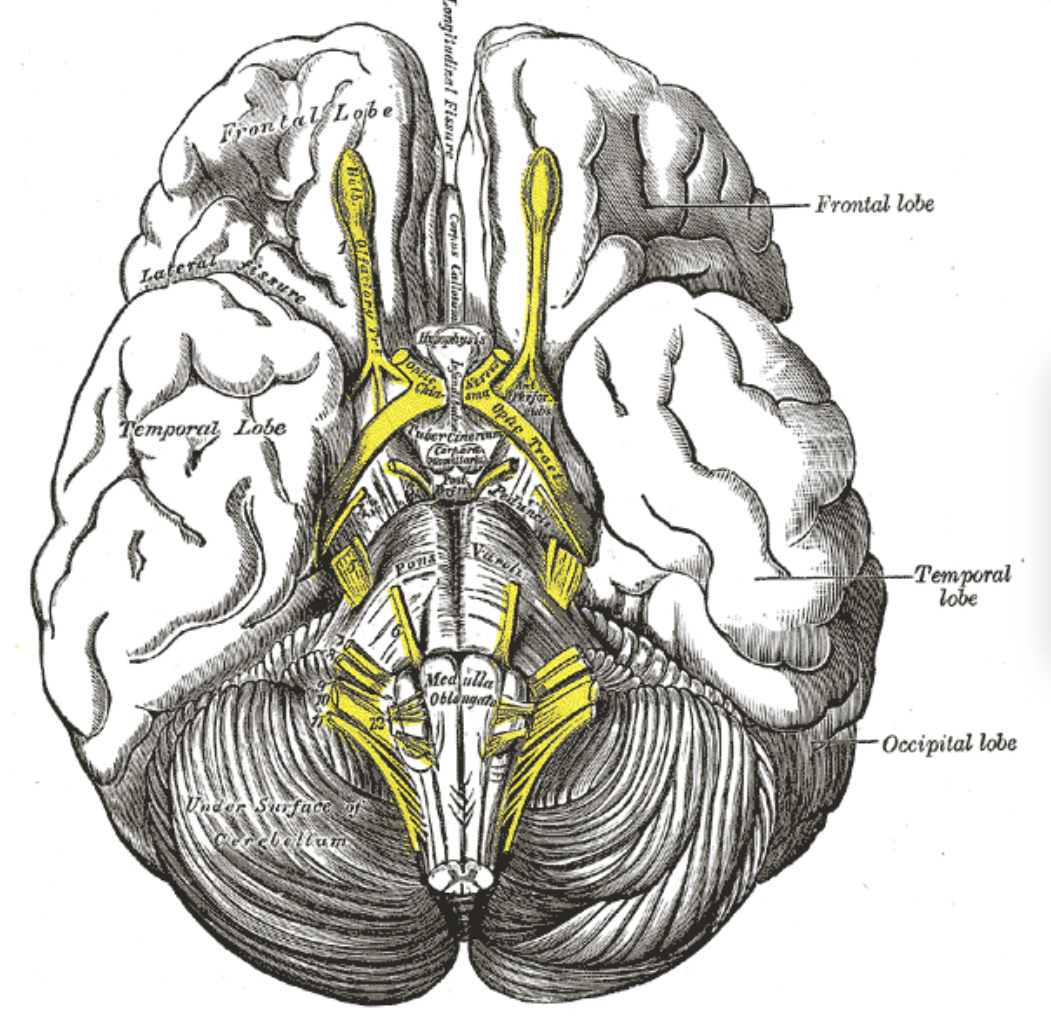
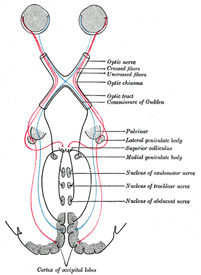
In mTBIs, FAS can emerge without significant structural lesions visible on imaging. Reports indicate that even minor head injuries might lead to FAS, with functional or metabolic brain changes undetected by standard imaging techniques. For instance, abnormal functions in specific brain regions, such as the left dorsolateral inferior frontal gyrus and caudate nucleus, have been implicated.
Overall, the occurrence of FAS in both FNDs and post-mTBI contexts underscores the complexity of this speech disorder and the need for integrated diagnostic and therapeutic approaches. The studies reviewed suggest that functional and metabolic assessments, alongside behavioural interventions, are crucial for understanding and managing FAS effectively.
Foreign Accent Syndrome Read Post »