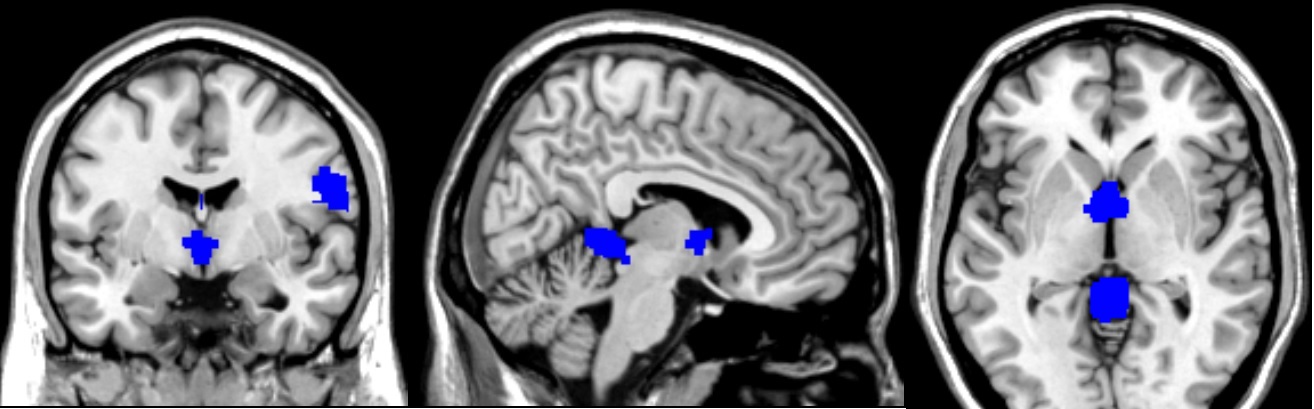
Functional neurological disorders (FNDs) present a diagnostic challenge due to the absence of definitive biomarkers. This synthesis of current research explores the potential biomarkers for FNDs, aiming to enhance diagnostic accuracy and treatment efficacy. Cortisol levels have been investigated as state, trait, and prognostic biomarkers, reflecting the stress response and potential chronic alterations in hypothalamic-pituitary-adrenal axis functioning in FND patients[1]. Whole-body cryostimulation (WBC) has been proposed as an adjuvant treatment, with a case report demonstrating improvements in body composition, hematological biomarkers, and physical performance, suggesting physiological responses to WBC as potential biomarkers for treatment efficacy[2]. Vitamin B12 deficiency, often resulting from nitrous oxide misuse, has been identified as a consistent feature in hospital admissions for neurological disorders, indicating the importance of metabolic biomarkers in patient management[3]. Functional near-infrared spectroscopy (fNIRS) has been utilized to derive objective hemodynamic biomarkers, with machine learning algorithms demonstrating high accuracy in classifying neuropsychiatric disorders, underscoring the potential of fNIRS in the objective diagnosis of FNDs[4]. Additionally, glutamatergic dysfunction, neuroplasticity, and redox status in peripheral blood have been explored as potential biomarkers for motor conversion disorders, a subtype of FNDs[5]. This body of research signifies a shift towards identifying unfeignable biomarkers that could unravel the complex etiology of FNDs and guide more targeted interventions[6][7].