The intricacies of brain pathology associated with concussion history are becoming increasingly significant in the medical field, particularly as we deepen our understanding of the long-term effects of head injuries. Concussions, especially those incurred through contact sports or repeated trauma, have been linked to a range of disabling symptoms that can severely impact an individual’s quality of life. This exploration delves into the complexities of these associations, shedding light on the broader implications for diagnosis, treatment, and prevention.
A concussion is not just a momentary lapse in function; it is a mild form of traumatic brain injury that can have profound and lasting effects. The relationship between repeated concussions and subsequent brain pathology is complex, encompassing a variety of symptoms and conditions that extend beyond what might be expected from individual instances of head trauma.
One of the key areas of focus in recent research has been on the variety of clinical symptoms observed in individuals with a history of repeated concussions. These symptoms can be neurological, such as headaches or dizziness; psychiatric, including depression and anxiety; and physical, like chronic pain. The severity and duration of these symptoms can vary widely, making it challenging to predict outcomes and tailor interventions effectively.
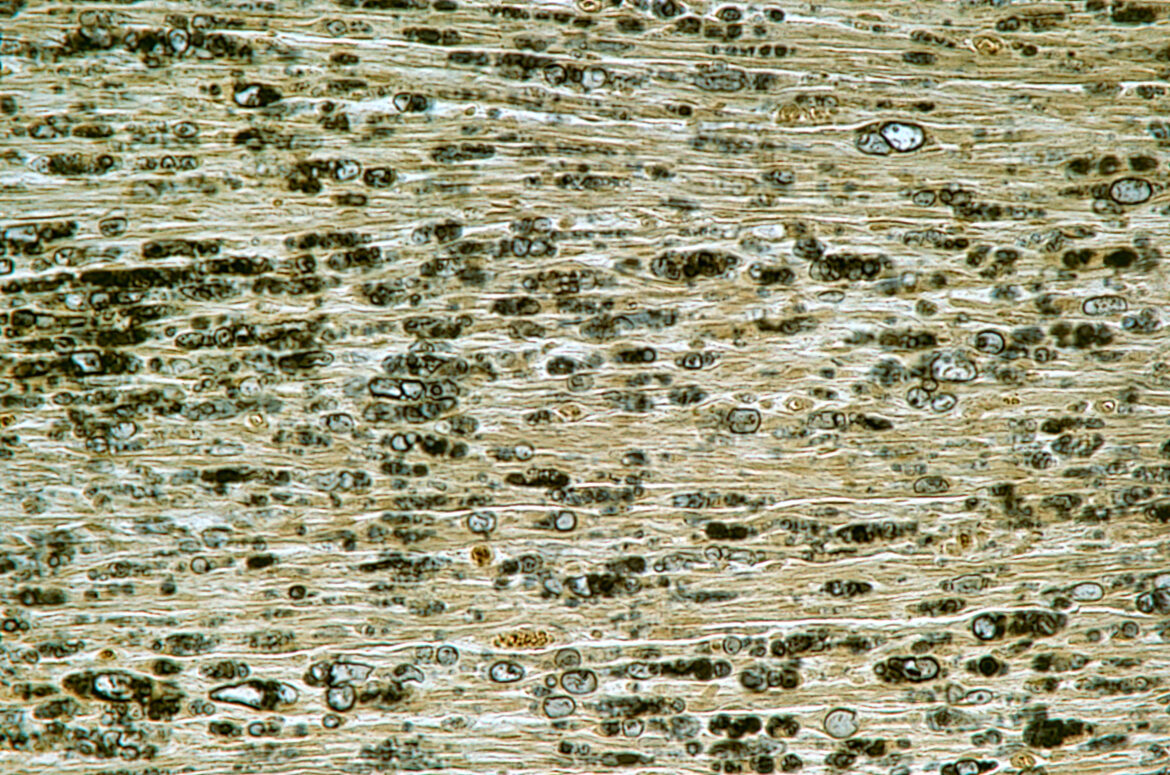
In addition to symptomatic concerns, the underlying neuropathological changes associated with concussions are of significant interest. These changes can include, but are not limited to, chronic traumatic encephalopathy (CTE), a condition historically associated with repeated head impacts. However, the spectrum of neuropathology is broad, with some individuals displaying evidence of other neurodegenerative diseases or mixed pathologies, such as Alzheimer’s disease, in the absence of significant CTE pathology. This suggests a multifactorial nature of brain injury outcomes, with various mechanisms contributing to the observed clinical manifestations.
An intriguing aspect of concussion-related brain pathology is the role of DNA damage. Emerging evidence indicates that DNA damage, particularly in certain areas of the brain, may correlate with both the history of concussion and the severity of clinical symptoms. This finding expands the scope of potential biomarkers and mechanisms of injury to be considered in the context of concussion history, beyond the proteinopathies traditionally associated with neurodegeneration.
The implications of these findings are vast for medical professionals. They underscore the importance of a comprehensive approach to managing individuals with a history of concussion, one that considers the broad spectrum of potential outcomes. It encourages healthcare providers to look beyond the conventional paradigms of concussion effects, exploring a wider array of diagnostic markers and therapeutic targets.
Furthermore, this knowledge emphasizes the critical need for personalized medicine in the treatment of concussion-related conditions. Understanding the diverse pathways through which concussions can affect brain health is key to developing targeted interventions that can mitigate the long-term impacts of head injuries.
In conclusion, the relationship between concussion history and brain pathology is characterized by a high degree of complexity, involving a wide range of clinical symptoms and underlying mechanisms. As research in this area continues to evolve, it will undoubtedly provide valuable insights that can inform more effective strategies for prevention, diagnosis, and treatment, ultimately improving the prognosis for individuals affected by concussion-related brain pathology.
Literature- further reading:
- McKee, A. C., Stein, T. D., Nowinski, C. J., Stern, R. A., Daneshvar, D. H., Alvarez, V. E., … & Cantu, R. C. (2013). The spectrum of disease in chronic traumatic encephalopathy. Brain, 136(1), 43-64. This seminal paper provides a comprehensive overview of chronic traumatic encephalopathy (CTE) in athletes and veterans, detailing the neuropathological features and potential impact of repeated head trauma.
- Gavett, B. E., Stern, R. A., & McKee, A. C. (2011). Chronic traumatic encephalopathy: A potential late effect of sport-related concussive and subconcussive head trauma. Clinics in sports medicine, 30(1), 179-xi. This review discusses the clinical, pathological, and epidemiological aspects of CTE, offering insights into the long-term consequences of sport-related head injuries.
- Gardner, R. C., Yaffe, K. (2015). Epidemiology of mild traumatic brain injury and neurodegenerative disease. Molecular and Cellular Neuroscience, 66, 75-80. This article explores the epidemiological link between mild traumatic brain injury, including concussions, and the risk of developing neurodegenerative diseases later in life.
- Johnson, V. E., Stewart, W., & Smith, D. H. (2012). Axonal pathology in traumatic brain injury. Experimental neurology, 246, 35-43. This research paper delves into the axonal injury mechanisms that occur in traumatic brain injury (TBI), discussing their implications for understanding the pathology and potential therapeutic targets.
- Tagge, C. A., Fisher, A. M., Minaeva, O. V., Gaudreau-Balderrama, A., Moncaster, J. A., Zhang, X. L., … & Goldstein, L. E. (2018). Concussion, microvascular injury, and early tauopathy in young athletes after impact head injury and an impact concussion mouse model. Brain, 141(2), 422-458. This study provides evidence of the connection between concussion, microvascular injury, and the early development of tauopathy, underscoring the complex pathology that can arise from head impacts.