Introduction
Functional Neurological Disorder (FND) presents a unique challenge in neurology and psychiatry due to its complex nature and the absence of clear organic causes for the symptoms. Unlike other neurological conditions, the symptoms of FND, such as motor, sensory, or cognitive disturbances, do not stem from deliberate actions and vary widely in severity. This article explores how medical professionals can differentiate FND from cases of malingering or feigning, where symptoms are intentionally produced.
Understanding FND
FND, formerly known as conversion disorder, is characterized by significant neurological symptoms that lack an identifiable physical origin. The diagnosis relies heavily on clinical evaluation and the exclusion of other medical or psychiatric conditions. Treatment usually involves a multidisciplinary approach, combining medical management, psychotherapy, and supportive interventions.
Advances in Diagnostic Approaches
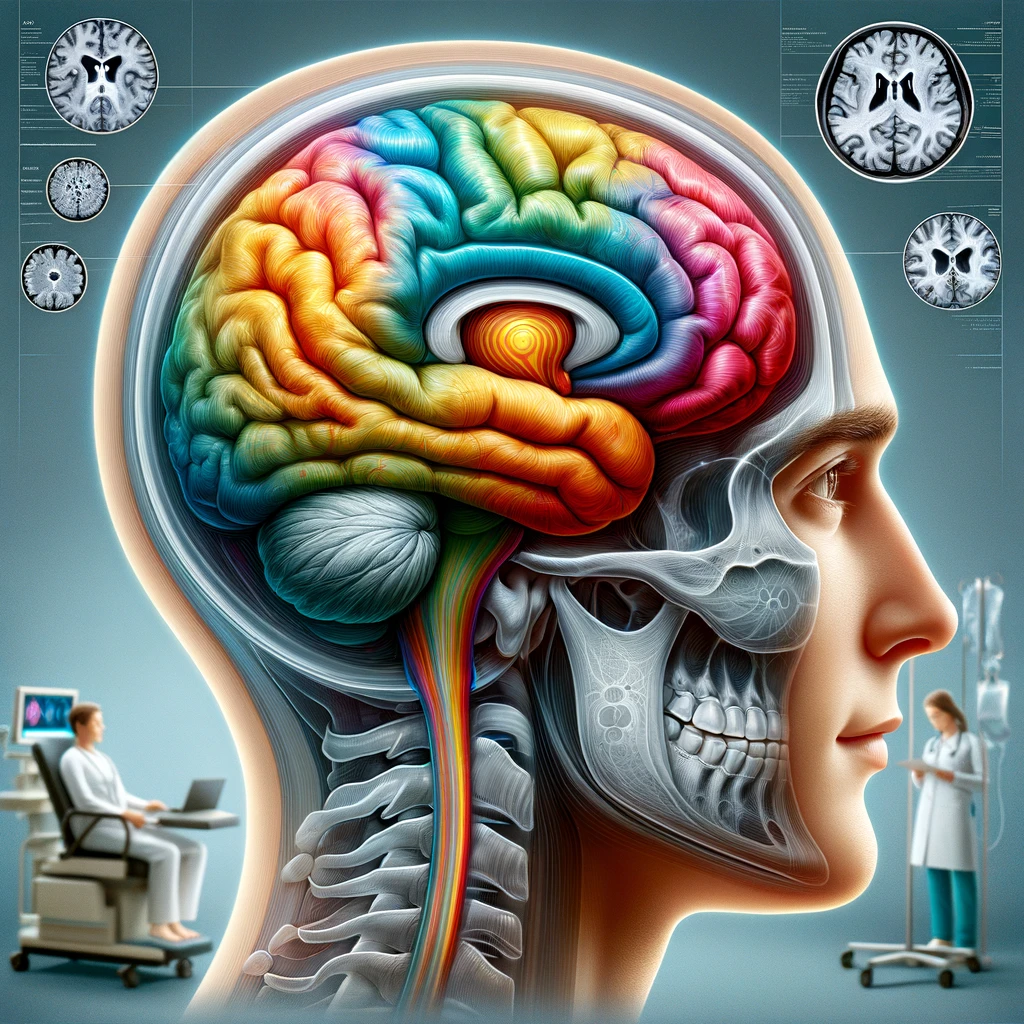
Recent advances in neuroimaging have played a crucial role in enhancing our understanding of FND. These imaging techniques help reveal the underlying neural mechanisms associated with the disorder, which are crucial for distinguishing FND from malingering or feigning. Neuroimaging can show specific patterns that are consistent with FND, differentiating them from those found in individuals who might be simulating symptoms.
Differentiating FND from Malingering or Feigning
The differentiation between FND and malingering or feigning hinges on the intention behind symptom presentation. Malingering involves the intentional production of symptoms for external gains, such as financial compensation or avoidance of duty. Feigning, similarly, involves deliberate symptom production but without the external incentives typically seen in malingering.
Clinical Interviews and Observations: Detailed clinical interviews and careful observation of symptom presentation over time are vital. Inconsistencies in reported symptoms versus observed behaviors can be a significant indicator of feigning or malingering.
Psychological Testing: Psychometric tests designed to detect deception or symptom exaggeration can be useful.
Consistency Across Evaluations: Consistency in symptom presentation across different times and settings is a key characteristic of FND. In contrast, individuals who are malingering or feigning often display variability that correlates with situational changes, such as increased observation or direct examination.
Response to Treatment: Patients with FND typically show some improvement with appropriate psychological and rehabilitative therapies. In contrast, those feigning or malingering might not demonstrate real improvement or could selectively respond only when it benefits their desired outcome.
Neuroimaging and Physiological Testing: While not definitive on their own, neuroimaging and other physiological tests can support a differential diagnosis. These tools can detect discrepancies in brain activity and bodily responses that are inconsistent with reported symptoms but aligned with known patterns of FND.
Ethical Considerations and Clinical Judgment
Accurately differentiating between FND and malingering or feigning requires not only technical knowledge and diagnostic skills but also careful ethical consideration. False accusations of malingering can harm patient-provider trust and impact the quality of care. Similarly, overlooking potential malingering can lead to inappropriate treatment plans and wasted resources. Therefore, the use of objective data combined with clinical expertise and ethical sensitivity is crucial.
Conclusion
Distinguishing FND from malingering or feigning remains a complex challenge in clinical practice. It requires a multifaceted approach that includes comprehensive clinical evaluations, advanced diagnostic tools, and a deep understanding of patient history and behavior. By employing thorough and ethically guided diagnostic practices, healthcare professionals can more accurately identify genuine cases of FND, ensuring that patients receive the appropriate care and management they need.
References–further reading
Mavroudis, I., Kazis, D., Kamal, F.Z., et al. (2024). Understanding Functional Neurological Disorder: Recent Insights and Diagnostic Challenges. Int. J. Mol. Sci., 25, 4470.