Traumatic brain injury (TBI) is recognized as a major global health concern, with an annual incidence of around 69 million cases worldwide. Once considered a static event with limited consequences beyond the acute phase, it is now widely accepted that TBI can have long-lasting effects on brain function, leading to progressive neurodegeneration and increased risk of dementia. Research indicates that TBI may account for a significant proportion of dementia cases, including Alzheimer’s disease (AD), Parkinson’s disease (PD), and chronic traumatic encephalopathy (CTE). This article aims to provide a comprehensive review of the mechanisms linking TBI to dementia, with an emphasis on the role of neuroimaging, biomarkers, and clinical trials.
The Epidemiology of Dementia Post-TBI
TBI and All-Cause Dementia
Multiple studies have confirmed that TBI increases the risk of all-cause dementia. A meta-analysis of more than two million individuals found that the overall risk of dementia was elevated by 1.6 times following TBI. Additionally, studies involving military veterans and large population-based cohorts have shown that the risk persists for decades after injury, with moderate-to-severe TBI carrying an even higher risk of dementia compared to mild TBI. It is estimated that TBI may account for 5-15% of all dementia cases globally .
Alzheimer’s Disease After TBI
Alzheimer’s disease is the most frequently studied form of dementia associated with TBI. Research has demonstrated that individuals with a history of TBI have approximately 1.5 times the risk of developing AD compared to those without TBI. Neuropathological studies have revealed that amyloid plaques, a hallmark of AD, are commonly found in the brains of individuals with TBI, particularly in men. Moreover, TBI may lead to an earlier onset of AD, with some studies reporting an average reduction in the age of onset by 3.6 years for those with a history of TBI .
Parkinson’s Disease and TBI
Parkinson’s disease (PD) is another neurodegenerative condition that shows an increased incidence following TBI. Studies indicate that individuals with a history of moderate-to-severe TBI have up to a 1.83 times higher risk of developing PD, while those with a history of mild TBI are also at an elevated risk. Repeated mild TBI, such as that sustained by athletes, has historically been associated with parkinsonism, leading to a syndrome known as “dementia pugilistica” or “Punch Drunk” syndrome .
Chronic Traumatic Encephalopathy (CTE)
Chronic traumatic encephalopathy (CTE) has attracted substantial attention in recent years, particularly in relation to athletes who sustain repeated head trauma. CTE is characterized by the deposition of hyperphosphorylated tau in specific regions of the brain, particularly in perivascular areas and deep cortical sulci. The pathological features of CTE overlap with other neurodegenerative diseases like Alzheimer’s but have distinct characteristics, including the unique shape and spread of tau deposits.
While CTE is currently only diagnosed postmortem, it presents a range of cognitive, emotional, and behavioral symptoms during life, such as memory impairment, aggression, and depression. Establishing clinical diagnostic criteria for CTE remains a challenge due to its symptomatic overlap with the direct effects of TBI and other dementias .
Mechanisms Linking TBI to Neurodegeneration
Diffuse Axonal Injury and Proteinopathies
One of the key mechanisms by which TBI leads to neurodegeneration is through diffuse axonal injury (DAI). DAI is characterized by the shearing of axons during the injury, which disrupts the normal function of the cytoskeleton and microtubules within neurons. This disruption leads to the buildup of pathological proteins, including tau and amyloid-beta, both of which are associated with Alzheimer’s disease and CTE. These proteinopathies can spread across the brain, potentially through prion-like mechanisms, leading to progressive neurodegeneration over time .
Chronic Inflammation and Microglial Activation
Inflammation plays a significant role in the progression of neurodegeneration following TBI. The brain’s immune cells, microglia, become activated in response to injury, and while this response initially serves to repair damaged tissue, chronic microglial activation can contribute to long-term neuronal damage and brain atrophy. Persistent inflammation may interfere with the brain’s ability to clear neurotoxic proteins like amyloid-beta and tau, exacerbating their accumulation and spread .
Vascular Damage and Blood-Brain Barrier Disruption
TBI can also lead to vascular damage, contributing to neurodegeneration through blood-brain barrier (BBB) disruption. In the acute phase following injury, the BBB becomes more permeable, allowing inflammatory molecules and immune cells to enter the brain. Over time, chronic vascular damage and impaired clearance of neurotoxic proteins may increase the risk of neurodegenerative diseases .
Diagnostic Tools: Imaging and Biomarkers
Neuroimaging
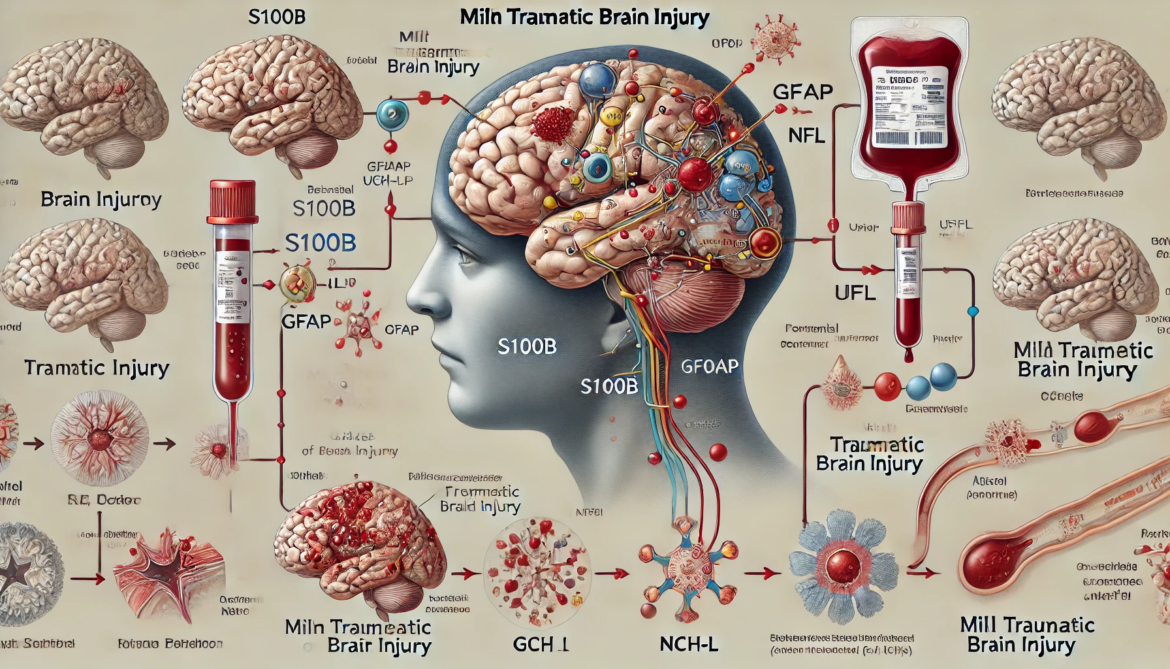
Advances in neuroimaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), have greatly improved our ability to detect neurodegeneration after TBI. MRI provides detailed insights into brain atrophy and white matter integrity, while PET imaging allows for the visualization of amyloid-beta and tau deposits in the brain.
Fluid Biomarkers
In addition to imaging, fluid biomarkers have emerged as valuable tools for diagnosing and monitoring neurodegeneration following TBI. Proteins such as neurofilament light (NFL) are released into the blood and cerebrospinal fluid (CSF) following axonal damage. Elevated levels of NFL in the chronic phase of TBI have been correlated with progressive brain atrophy and cognitive decline.
Clinical Trials and Therapeutic Approaches
Given the growing recognition of TBI as a risk factor for neurodegeneration, there is an urgent need for clinical trials to evaluate potential treatments. Biomarkers such as brain atrophy rates and NFL levels offer sensitive and specific endpoints for clinical trials. By identifying patients at high risk of neurodegeneration using these biomarkers, researchers can enrich trial populations and reduce the number of participants required to detect meaningful treatment effects.
Conclusion
The link between TBI and dementia is well-established, with mechanisms involving axonal injury, chronic inflammation, and vascular damage contributing to the progression of neurodegeneration. Advances in neuroimaging and biomarker research have improved our ability to diagnose and monitor post-traumatic dementia, while ongoing clinical trials hold promise for the development of effective neuroprotective treatments. As research in this field continues to evolve, it is essential to refine diagnostic criteria for post-traumatic dementia and implement targeted interventions to reduce the long-term impact of TBI on brain health.