Research Objectives
The primary aim of the Boston University Alzheimer’s Disease Research Center Clinical Core is to enhance the understanding of post-traumatic Alzheimer’s disease and related dementias through a structured research framework. By focusing on the intersection of trauma and neurodegeneration, the center seeks to identify specific mechanisms through which traumatic events may influence the onset and progression of Alzheimer’s disease. This involves investigating the biological, psychological, and social factors that could mediate this relationship, thereby contributing to the broader field of dementia research.
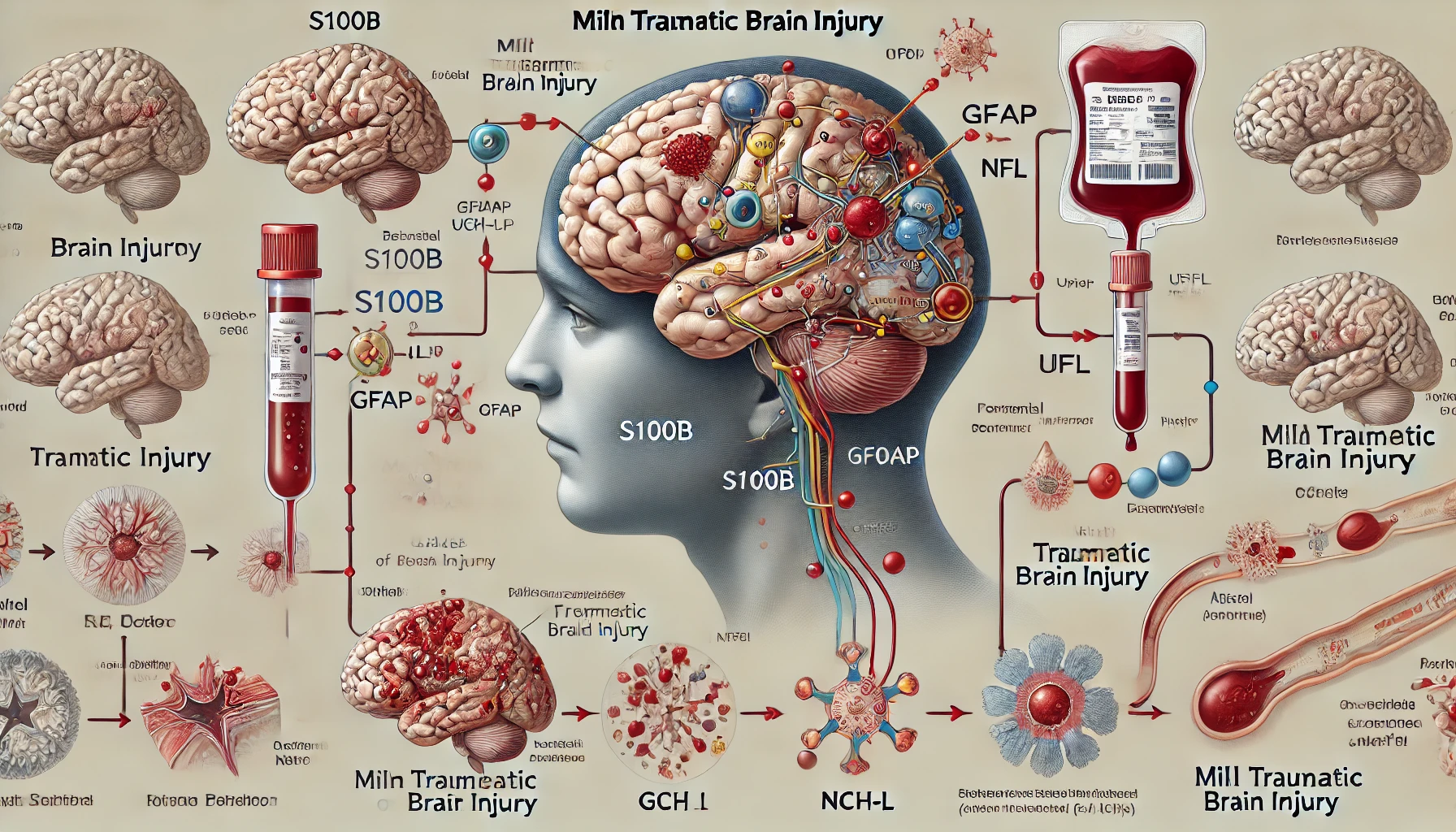
An important objective is to explore the role of neuroinflammation and other pathophysiological changes following an injury, such as traumatic brain injury (TBI). Research has indicated that individuals with a history of TBI are at an increased risk for cognitive decline and Alzheimer’s disease, but the precise pathways and timelines remain unclear. By utilizing advanced neuroimaging techniques and biomarker analysis, the center aims to delineate how these factors interact over time, ultimately leading to targeted interventions.
Additionally, the center is committed to understanding the psychosocial impacts of post-traumatic conditions on patients and their caregivers. This includes studying the effects of cognitive impairments on daily functioning and quality of life, thus ensuring that research is not only focused on biological aspects but also on the lived experiences of those affected. Another key objective is to develop strategies for early detection of Alzheimer’s disease in at-risk populations, which can lead to earlier therapeutic interventions and better management of symptoms.
Consequently, the research will support the identification of potential therapeutic targets, providing a foundation upon which new treatments can be developed. These objectives align with the center’s mission to foster collaboration among multidisciplinary teams, ensuring a comprehensive approach to tackling the complexities of post-traumatic Alzheimer’s disease and related dementias.
Participant Recruitment and Selection
The success of the Boston University Alzheimer’s Disease Research Center Clinical Core relies significantly on its ability to strategically recruit and select participants for its studies. This process is designed to ensure a representative sample that not only reflects the diversity of the general population but also captures the nuances of individuals who have experienced trauma and are at risk for developing Alzheimer’s disease and related dementias.
To begin with, the recruitment strategy encompasses various community outreach initiatives aimed at raising awareness about the research center’s goals and the importance of participation in dementia research. Collaborations with local hospitals, community organizations, and veterans’ groups play a vital role in disseminating information and encouraging individuals who have sustained traumatic brain injuries or those exhibiting cognitive decline to consider taking part in the studies. These partnerships foster trust and ensure that recruitment efforts reach underrepresented populations who may not have easy access to research opportunities.
Potential participants are screened through a multi-step process that includes initial assessments via phone interviews and in-person evaluations. Key inclusion criteria are established based on the specific research objectives, such as a confirmed history of traumatic brain injury, cognitive assessments indicating early stages of dementia, or other relevant health conditions. This rigorous selection process ensures that the sample accurately reflects the target population, which is essential for the validity of the research findings.
Ethical considerations are paramount throughout the recruitment and selection process. Informed consent is obtained from all participants, ensuring they fully understand the nature of the research, the procedures involved, potential risks, and their right to withdraw at any time without any repercussions. The center prioritizes transparency and respect for participant autonomy, thereby fostering an environment of open communication.
In addition, diversity in age, gender, ethnicity, and socioeconomic status among participants is actively sought. This diversity is crucial for examining how different demographic factors may influence the progression of Alzheimer’s disease and the impact of traumatic experiences. The inclusion criteria are designed to allow for a broad spectrum of participants, enabling researchers to explore variability in biological markers and symptoms across different groups.
The identification of caregivers is also an integral part of participant recruitment, as their involvement can provide complementary perspectives on the challenges faced by individuals with dementia. The experiences of both patients and caregivers are crucial, as they highlight the social dimensions of navigating post-traumatic distress and cognitive decline.
Finally, ongoing assessments and follow-ups with participants are conducted to ensure continued engagement and gather valuable longitudinal data. This process not only helps maintain participant involvement throughout the study but also provides insights into changes in cognitive function and the long-term effects of trauma on dementia progression. By systematically approaching participant recruitment and selection, the Boston University Alzheimer’s Disease Research Center Clinical Core aims to generate robust and impactful research findings that can inform future interventions and ultimately improve outcomes for individuals at risk for Alzheimer’s disease and related dementias.
Data Collection and Analysis
The ongoing research at the Boston University Alzheimer’s Disease Research Center Clinical Core employs a multifaceted approach to data collection and analysis, which is pivotal in drawing reliable connections between traumatic brain injury (TBI), neurodegeneration, and the development of Alzheimer’s disease and related dementias. The core methodology encompasses quantitative, qualitative, and mixed-methods approaches tailored to capture a comprehensive perspective on the intricate relationships among neurological, psychological, and social factors.
Data collection begins with the utilization of advanced neuroimaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), which allow researchers to visualize brain structures and metabolic activity in participants. These imaging modalities are crucial for identifying biomarkers of neuroinflammation and neurodegeneration following trauma. The interpretation of these scans provides essential insights into how structural and functional changes in the brain correlate with cognitive decline and the onset of Alzheimer’s disease.
In addition to neuroimaging, the center collects a variety of biological samples, including blood, cerebrospinal fluid (CSF), and genetic material. These samples are analyzed for biomarkers associated with inflammatory processes and tau pathologies, which are key indicators of Alzheimer’s disease progression. By correlating these biological markers with clinical data, researchers can explore potential pathways linking TBI to neurodegenerative processes.
Cognitive assessments form an integral part of the data collection framework. Standardized tests and evaluations, such as the Mini-Mental State Examination (MMSE) and the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog), are employed to measure cognitive function across participants. These assessments are conducted at baseline and at follow-up intervals, allowing for the tracking of cognitive changes over time in relation to traumatic events and the associated biological changes.
Qualitative data is gathered through interviews and questionnaires aimed at understanding participants’ personal experiences with trauma and dementia-related symptoms. This subjective data is invaluable as it captures the psychosocial impacts on both patients and caregivers. The center employs thematic analysis to identify common themes and narratives, which provide richer context to the quantitative findings and highlight the lived experiences of individuals navigating the challenges associated with post-traumatic cognitive decline.
Data analysis is facilitated through robust statistical methodologies that ensure the reliability and validity of findings. Advanced statistical software programs are employed to perform various analyses, including regression models that assess the relationships between traumatic injury, biological markers, cognitive decline, and various demographic factors. These analyses aim to establish patterns and predictive factors associated with Alzheimer’s disease, thereby yielding insights that are critical for developing targeted interventions.
Furthermore, the center emphasizes the integration of multidisciplinary expertise in data interpretation. Collaborative efforts involving neurologists, psychologists, and biostatisticians ensure a holistic view of the data, allowing for a comprehensive understanding of the interactions between trauma, neurobiology, and cognitive health. This collaboration fosters a thorough evaluation of potential confounding variables and enhances the overall robustness of the research design.
Ethical considerations remain at the forefront during data collection and analysis. Respecting participant confidentiality and ensuring data security are paramount, and all analyses are conducted in adherence to ethical guidelines outlined by the Institutional Review Board (IRB). This commitment to ethical research practices underpins the integrity of the findings and the trust placed in the center by participants.
In summary, the data collection and analysis framework utilized by the Boston University Alzheimer’s Disease Research Center Clinical Core is designed to facilitate a deep understanding of the complex interplay between trauma and Alzheimer’s disease. By employing a combination of advanced neuroimaging, biomarker analysis, cognitive assessments, and qualitative interviews, the center aims to uncover insights that will inform future research directions and potential therapeutic approaches.
Future Directions
The Boston University Alzheimer’s Disease Research Center Clinical Core is poised for significant growth and impact in addressing the complexities of post-traumatic Alzheimer’s disease and related dementias. In the near future, the center aims to expand its research scope, employing innovative methodologies and interventions that build on its foundational objectives.
One primary direction includes the integration of longitudinal studies to deepen the understanding of how trauma influences cognitive decline over time. By following participants for extended periods, researchers will be able to observe the progression of neurodegenerative changes and their correlation with traumatic events. This longitudinal approach will not only enhance knowledge about the timing and nature of these relationships but also aid in identifying critical windows for therapeutic intervention.
The development and validation of new biomarkers represent another future avenue of research. The center is exploring cutting-edge technologies, such as liquid biopsies and advanced genetic analysis, to discover novel biomarkers that could indicate early pathological changes associated with Alzheimer’s disease. These biomarkers will be essential in designing personalized treatment plans that could mitigate the progression of the disease post-trauma.
Additionally, there is a strong emphasis on community-based participatory research (CBPR) to elevate patient and caregiver voices within the research process. Engaging stakeholders in the design and implementation phases will ensure that the research addresses their most pressing concerns and needs. This involvement will enhance the relevance and applicability of findings and promote greater awareness and acceptance of research participation among diverse populations.
Expanding collaborations with other research institutions and healthcare organizations is also a vital goal. By forming partnerships with experts across various fields, such as genetics, psychology, and neuroimaging, the center aims to foster interdisciplinary research that enriches insights into trauma and neurodegeneration. Such collaborations will facilitate access to larger, more diverse participant pools, enhancing the generalizability of findings.
The utilization of advanced artificial intelligence (AI) and machine learning techniques will be a transformative aspect of future research endeavors. These technologies can analyze large datasets, revealing complex patterns that may not be immediately apparent through traditional analytical methods. By harnessing AI, researchers at the center will be able to predict outcomes based on genetic, biomarker, and clinical data, which could lead to groundbreaking preventive strategies for at-risk populations.
Furthermore, there will be an increased focus on developing and testing interventions aimed at both care for individuals affected and support for caregivers. Innovative programs like cognitive training, physical rehabilitation, and mindfulness therapies will be explored to mitigate cognitive decline and improve quality of life. Research will emphasize not only on the clinical efficacy of these interventions but also on their economic viability and accessibility for families.
Ethical considerations will remain central as the center seeks to expand its research capabilities. Ensuring participant safety, informed consent, and data integrity will be paramount, particularly given the sensitive nature of post-traumatic conditions and cognitive decline. Transparency in research practices will enhance community trust and participation.
Through these multifaceted directions, the Boston University Alzheimer’s Disease Research Center Clinical Core is committed to advancing the understanding of post-traumatic Alzheimer’s disease and implementing changes that will lead to tangible benefits for individuals affected and their families. Their endeavor will not only contribute to academic knowledge but also provide pathways to improve public health outcomes in aging populations.