Dissociation and Seizure Classification
Dissociation is a complex psychological phenomenon characterized by disruptions in the normal integration of consciousness, memory, identity, and perception. In the context of seizures, particularly functional or dissociative seizures, the classification of these episodes poses significant challenges within clinical practice. These seizures can manifest in various forms, leading to potential misdiagnosis or the overlooking of critical underlying neurobiological processes. The classification framework primarily used is based on the International League Against Epilepsy (ILAE) criteria, which segments seizures into focal and generalized categories. However, dissociative seizures often do not fit neatly into these established categories, leading to complications in identifying appropriate diagnostic and treatment pathways.
The differentiation between epileptic seizures and non-epileptic seizures, particularly dissociative seizures, remains a pressing clinical conundrum. Understanding the nuances of dissociative seizure presentations is essential for accurate diagnosis. For instance, while epileptic seizures typically feature observable brain activity changes on an electroencephalogram (EEG), dissociative seizures may present with similar clinical features but without corresponding ictal changes. This distinction emphasizes the necessity for rigorous clinical assessments, including thorough histories and possibly prolonged EEG monitoring, to avoid misdiagnosis and inappropriate management strategies.
Moreover, the psychological contexts surrounding dissociative seizures can significantly influence their manifestation and classification. Many patients experience these seizures in conjunction with trauma or stress, complicating their clinical picture. Such episodes may be mistaken for other neurological disorders, leading to misclassification and potential legal ramifications when untreated or mismanaged. For instance, in medicolegal contexts, an incorrect diagnostic label may affect personal injury claims or the status of fitness to work or drive, highlighting the importance of precise classification and understanding.
To advance the classification of dissociative seizures and enhance therapeutic approaches, ongoing research is necessary to elucidate the shared and diverging neurobiological mechanisms that underpin both functional and epileptic seizures. Clinicians must remain vigilant in their evaluations, applying both clinical acumen and established diagnostic criteria while remaining open to emerging findings in the field. Establishing clear diagnostic categories can facilitate more targeted treatment options and reduce the duration that patients may experience unmanaged symptoms.
Neurobiological Mechanisms Across the Lifespan
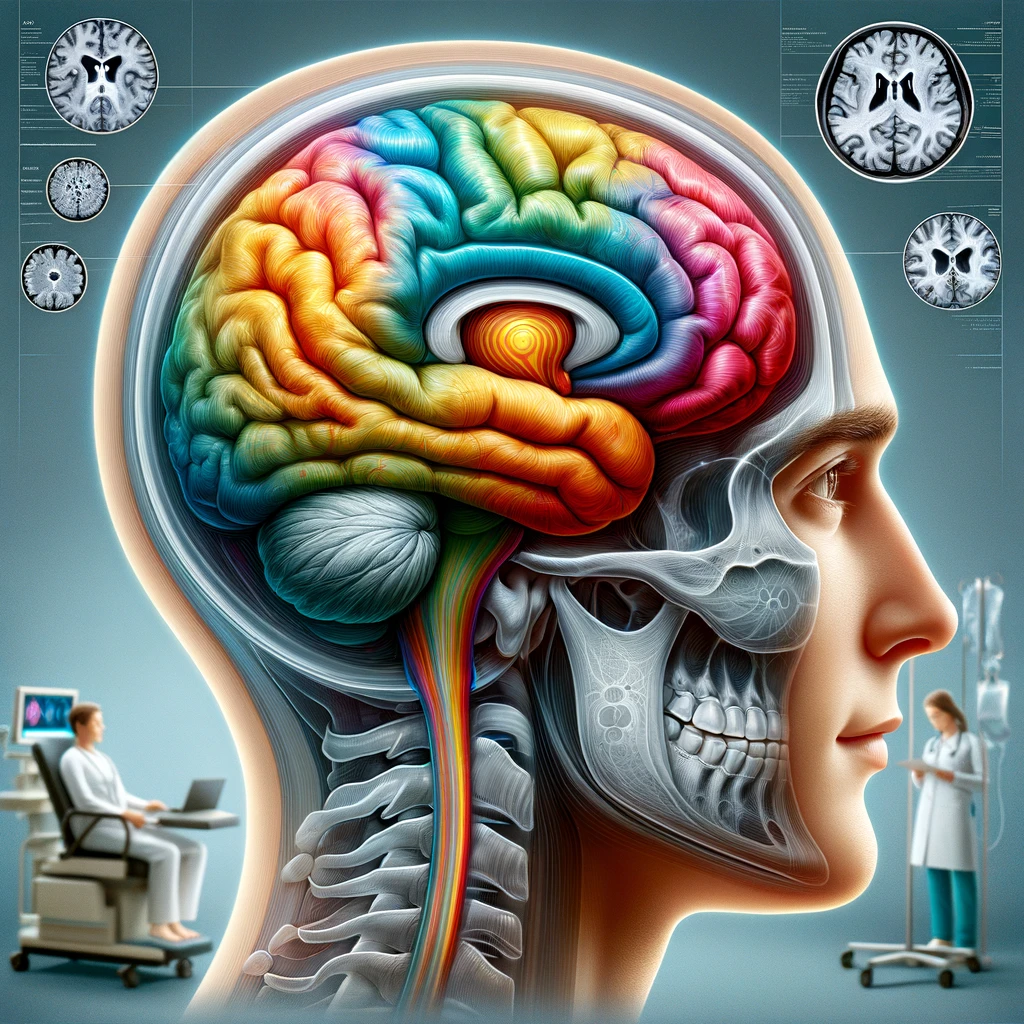
Neurobiological mechanisms underlying functional or dissociative seizures are complex and vary considerably across the lifespan, influenced by developmental changes and unique psychological profiles at different ages. Research indicates that these seizures involve dynamic interactions between the brain’s structural and functional systems, as well as psychosocial factors that differ significantly based on a patient’s age and life stage.
In the developing brain, particularly in children and adolescents, the neurobiological substrate of dissociation is often intertwined with the growing understanding of neurodevelopmental disorders. Functional seizures in younger populations may be particularly linked to stress responses, adverse childhood experiences, or early trauma. Neuroimaging studies reveal that childhood trauma can alter brain structures, such as the hippocampus and amygdala, key regions involved in emotional regulation and memory. These alterations may predispose young individuals to dissociative responses, which can manifest as seizures. It is essential for clinicians to consider these factors when assessing pediatric patients, as early recognition can prevent progression into chronic conditions and enhance therapeutic outcomes.
As individuals transition into adulthood, the neurobiological landscape continues to evolve. The prefrontal cortex, responsible for higher cognitive functions, undergoes maturation, which impacts emotional processing and regulation. Adults experiencing functional seizures often contend with significant psychological stressors, such as work-related pressures or personal relationships, which can trigger dissociative episodes. Neurologically, this demographic may exhibit changes such as altered connectivity patterns within the default mode network, which is associated with self-referential thought processes and is frequently disrupted in individuals with dissociative disorders. Understanding these underlying neurobiological changes can inform targeted therapeutic interventions that address both the psychological and physiological components of the seizures.
In older adults, the neurobiological correlates of dissociative seizures can be influenced by age-related cognitive decline, comorbid medical conditions, and changing psychosocial dynamics, including loss or isolation. The presence of neurodegenerative diseases, such as Alzheimer’s or Parkinson’s disease, can further obscure the picture, complicating both diagnosis and treatment. Research suggests that older adults may experience dissociative seizures in response to neurobiological deterioration combined with psychological stressors, such as grief or anxiety related to aging. Clinicians must adopt a holistic approach that considers the complex interplay of neurobiology and psychosocial factors, enabling appropriate diagnostic categorization and management strategies that cater to the individual’s unique needs.
From a clinical perspective, understanding these neurobiological mechanisms and their evolution across the lifespan is critical for effective patient management. Accurate assessment that takes into account age-related neurobiological changes, along with psychological history, can significantly improve diagnostic accuracy. This is especially relevant in medicolegal contexts, where misclassification of seizures can lead to inappropriate therapeutic decisions, disability determinations, and implications for driving or employment. By fostering a nuanced understanding of how these mechanisms evolve, clinicians can better equip themselves to recognize and treat patients effectively, minimizing the impact of both functional seizures and dissociative responses in their lives.
Impact on Patient Management
In managing patients with functional or dissociative seizures, a multifaceted approach is crucial for optimizing care and improving outcomes. Clinicians must focus on individualized treatment plans that address not only the seizure episodes themselves but also the underlying psychological and psychosocial factors contributing to the dissociative phenomena. Early and accurate diagnosis is paramount, as misdiagnosis can lead to inappropriate interventions, increased patient distress, and more complex clinical challenges. For instance, mistakenly treating a patient for epilepsy when they actually have dissociative seizures could result in unnecessary medication side effects and failure to address the root causes of their symptoms.
One essential component in the management of these patients is the implementation of education and empowerment strategies. Providing thorough explanations about the nature of functional seizures can alleviate patient anxiety and foster a greater understanding of their condition. Psychoeducation not only helps patients and their families comprehend the distinction between epileptic and dissociative seizures but also encourages active participation in their own care. Clinical engagement through cognitive-behavioral therapy (CBT) or tailored counseling can further help patients develop coping strategies for managing triggers and reducing the frequency of seizure episodes.
Furthermore, exploring psychological support mechanisms is vital. Given that many individuals experience dissociation in relation to trauma or stress, therapies that focus on trauma recovery—such as eye movement desensitization and reprocessing (EMDR) or somatic experiencing—may prove beneficial. These approaches can help patients process and integrate traumatic experiences, potentially reducing the incidence of dissociative seizures. In addition to therapy, mindfulness and relaxation techniques can serve as adjunct interventions, empowering patients with tools to manage stress, thereby decreasing the likelihood of seizure onset.
From a healthcare system perspective, collaboration among interdisciplinary teams is also critical. Neurologists, psychiatrists, psychologists, and primary care providers must work together to create comprehensive care plans that address the diverse needs of individuals with functional seizures. Coordinated care not only enables more holistic treatment but also ensures that all relevant factors—biological, psychological, and social—are considered and managed. This teamwork approach can facilitate smoother referrals to mental health services and streamline access to supportive resources.
In a medicolegal context, clear documentation of diagnostic processes, treatment plans, and patient progress is essential. This meticulous record-keeping can substantiate clinical decisions and protect against potential litigation issues that arise from misdiagnosis or insufficient care. For instance, in cases related to disability claims or fitness assessments, thorough documentation of a patient’s symptomatology and the rationale behind the chosen treatment pathway becomes critical. Such diligence ensures that patients receive appropriate care while safeguarding practitioners against legal repercussions.
Ultimately, enhancing patient management for individuals with dissociative seizures requires a holistic approach that encompasses accurate diagnosis, psychological support, interdisciplinary collaboration, and meticulous documentation. By addressing the complex interplay of factors that contribute to functional seizures, we can minimize their impact on patients’ lives and promote a more effective therapeutic process.
Future Research Directions
The trajectory of research into functional and dissociative seizures suggests a pressing need for enhanced understanding and elucidation of effective diagnostic and treatment methodologies. Investigating the prevalence and mechanisms of dissociative seizures across various populations offers an opportunity to refine existing knowledge and approaches. Future studies should prioritize longitudinal designs and large-scale, multicentric trials to capture a more comprehensive picture of these phenomena, particularly in diverse demographic groups. This would allow researchers to identify potential risk factors and the natural history of dissociative seizures, paving the way for preventive strategies.
Moreover, the integration of advanced neuroimaging techniques, such as functional MRI (fMRI) and positron emission tomography (PET), can illuminate the neural correlates associated with dissociative seizures. Understanding the brain networks involved in these episodes could facilitate the development of biomarkers for more precise diagnosis, distinguishing between functional seizures and traditional epilepsy. Continued exploration of how emotional and psychological states influence cortical activity offers avenues to understand the dynamic interplay between mental health and seizure presentations, which is crucial for individualized patient care.
Collaboration with mental health professionals cannot be overstated. Interdisciplinary studies focusing explicitly on the correlation between psychological trauma and the onset of dissociative seizures have the potential to unveil critical insights into treatment modalities. Research assessing the effectiveness of various psychotherapeutic interventions—ranging from trauma-focused cognitive-behavioral therapy to mindfulness-based stress reduction—could significantly enhance management protocols and patient outcomes. Implementing randomized controlled trials to gauge the efficacy of these therapies relative to traditional medical management strategies is essential for adapting treatment guidelines.
Furthermore, exploring the impact of societal and cultural factors on the perception and management of dissociative seizures warrants attention. Cultural competencies in healthcare can lead to better patient-provider communication, improve treatment adherence, and foster a more supportive environment for recovery. Focused research on how stigma and societal biases influence the experiences of patients with dissociative seizures can inform educational efforts aimed at healthcare professionals and the public, ultimately aiming to destigmatize these conditions.
Lastly, the use of technology in monitoring and diagnosing dissociative seizures presents a significant area for exploration. Wearable devices equipped with physiological monitoring capabilities may provide insights into the precursors of seizures, facilitating prompt intervention strategies. Incorporating artificial intelligence and machine learning algorithms for data analysis could enhance predictive modeling, offering clinicians tools to tailor preventive measures specific to individual patients’ patterns and triggers.
In the medicolegal realm, future research initiatives should also focus on the implications of improved diagnostic accuracy in mitigating legal disputes. As understanding of dissociative seizures expands, so too does the potential for more reliable assessments in contexts such as insurance claims, fitness for duty evaluations, and disability cases. Establishing clear guidelines based on robust evidence will help protect patient rights and ensure equitable access to care, while simultaneously safeguarding healthcare providers against litigation risks stemming from misdiagnosis.