Treatment Approaches
The management of Complex Regional Pain Syndrome (CRPS) and Functional Neurological Symptom Disorder (FNSD) in adolescents necessitates a comprehensive and multi-faceted approach tailored to the specific needs of the young patient. Various treatment modalities have been employed, each playing a critical role in alleviating symptoms and promoting recovery.
Physical therapy is a cornerstone in the treatment plan, emphasizing gradual reconditioning and strengthening of affected areas. A bespoke program often includes desensitization techniques to reduce pain perception and enhance mobility. Therapists frequently employ graded exposure strategies, aiming to slowly increase the patient’s tolerance for activities that may exacerbate pain. This method also aids in combating disuse atrophy, as the patient may initially avoid movement due to pain apprehension.
In conjunction with physical rehabilitation, cognitive-behavioral therapy (CBT) has shown promise in addressing the psychological dimensions associated with CRPS and FNSD. CBT can help patients develop coping mechanisms and modify maladaptive thought patterns related to pain and disability. By fostering a more adaptive mindset, adolescents are better equipped to engage with their rehabilitation, potentially leading to improved outcomes.
Medications also play a pivotal role in the management of these conditions. Common pharmacological treatments for CRPS may include anti-inflammatory drugs, anticonvulsants, and neuropathic pain agents, such as gabapentin. In some cases, opioids may be considered, although their use must be approached cautiously due to the risk of dependency, particularly in young patients. For FNSD, treatment may focus more on managing comorbid anxiety and depression, with a preference for non-addictive medications.
Additionally, interdisciplinary collaboration is imperative in the treatment of these complex conditions. Involving pain specialists, psychologists, physiatrists, and occupational therapists creates a holistic care environment that addresses both physical and psychological components. This team approach ensures that all aspects of the adolescent’s health are considered, leading to more effective management.
Furthermore, the integration of newer therapeutic interventions, such as mirror therapy and virtual reality, has begun to emerge as effective strategies in treating CRPS. These techniques exploit the brain’s neuroplasticity to retrain the brain’s perception of pain and limb function, thereby providing relief and promoting recovery.
Medico-legal considerations are also paramount, especially regarding the chronic nature of these conditions and their potential impact on the adolescent’s quality of life and schooling. It is essential for healthcare providers to document progress and treatment responses meticulously, as these records may play a significant role in any legal contexts that arise—in particular, issues related to disability claims or school accommodations.
In summary, an effective treatment strategy for CRPS and FNSD in adolescents incorporates a combination of physical rehabilitation, psychological support, medication management, and multidisciplinary collaboration, with ongoing evaluation and adjustment of the treatment plan being crucial to addressing this complex set of disorders.
Assessment Techniques
Accurately diagnosing Complex Regional Pain Syndrome (CRPS) and Functional Neurological Symptom Disorder (FNSD) in adolescents is paramount to developing an effective treatment plan. A comprehensive assessment involves utilizing a variety of techniques designed to understand the complexity of these disorders fully, integrating both subjective and objective measures.
Clinicians typically begin with a thorough medical history to capture the context surrounding the onset of symptoms. This narrative provides insights into any preceding events, such as physical trauma or emotional stressors, that may have contributed to the development of CRPS or FNSD. Additionally, assessing the adolescent’s psychosocial environment is crucial, as factors such as family dynamics, school stressors, and social interactions can influence both the presentation of symptoms and the recovery process.
Physical examination is vital. In cases of CRPS, the clinician looks for hallmark features such as changes in skin color, temperature, and swelling. These signs may help differentiate CRPS from other forms of pain syndromes. The evaluation may also include assessing the range of motion and the presence of allodynia or hyperalgesia, which are sensitivities to normally non-painful stimuli or heightened pain responses, respectively.
For FNSD assessment, clinicians often employ the use of diagnostic criteria, such as the DSM-5, while also utilizing functional neurological exams to observe the nature of symptoms during specific tasks. Various scoring systems can be employed to quantify functional impairments, including the Disability Rating Scale (DRS) or the Functional Independence Measure (FIM), which can help track progress over time and guide therapeutic interventions.
Additionally, psychometric assessments may provide valuable data concerning the psychosocial dimensions of pain. Tools such as the Beck Anxiety Inventory and the Child Depression Inventory facilitate understanding the emotional wellbeing of the adolescent. These assessments can reveal co-occurring mental health issues that may impact treatment efficacy and should be addressed concurrently.
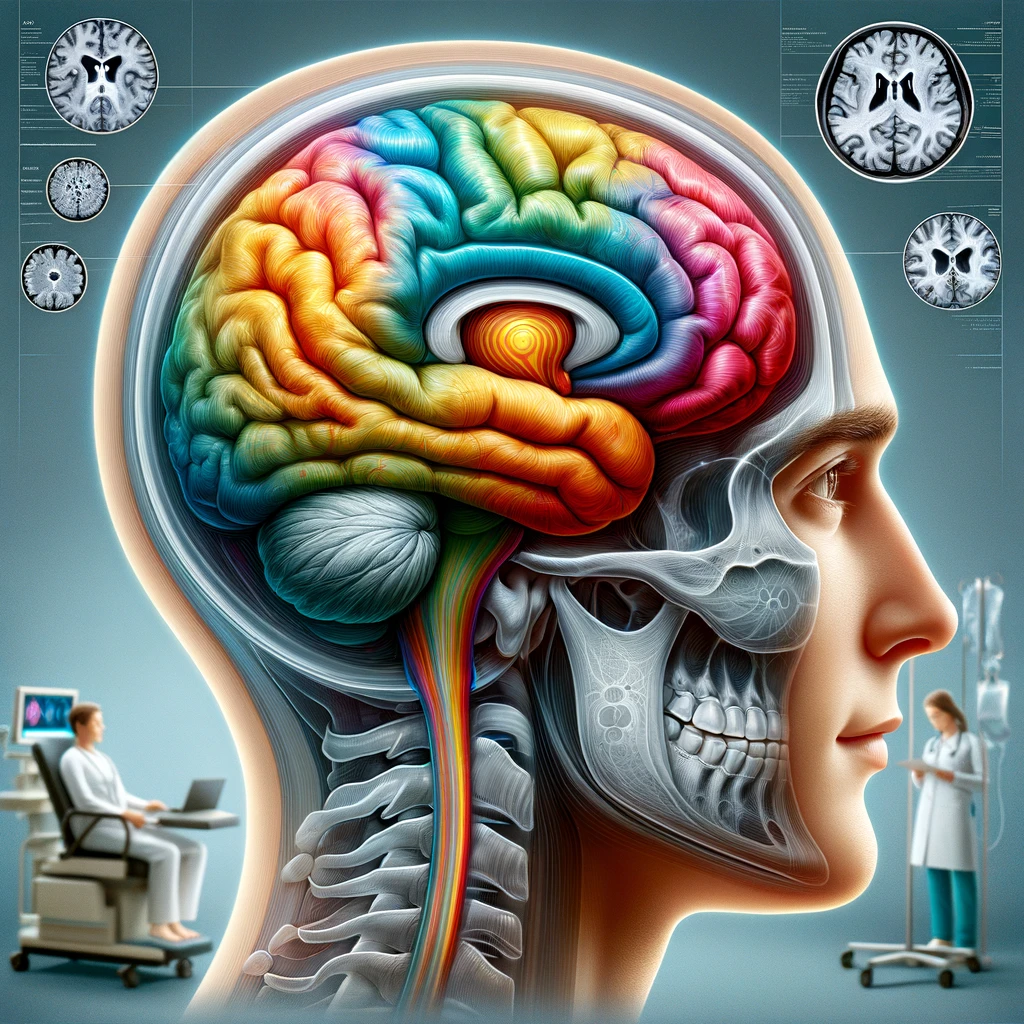
Neuroimaging techniques, including MRI or functional MRI, can complement clinical assessments by revealing patterns of brain activity associated with pain perception and symptoms. While these imaging modalities may not be diagnostic per se, they can provide insights into neural correlates of the patient’s experience and help guide rehabilitation strategies based on visual patterns of brain activation related to pain processing.
Collaboration among healthcare providers is crucial in assessing these multifaceted disorders. Multidisciplinary assessments involving pain specialists, psychologists, physical therapists, and other relevant professionals can create a holistic view of the patient’s challenges. Regular interdisciplinary meetings can ensure that assessment findings inform each team member’s approach, enhancing the individualized treatment plan.
From a medicolegal perspective, precise and documented assessments are critical. Thorough records of clinical evaluations add credence to treatment decisions and can be central in legal cases involving disability claims or educational modifications. Ensuring accurate documentation not only aids in patient care but also provides essential evidence in potential disputes arising from the adolescent’s condition.
In essence, the assessment of CRPS and FNSD in adolescents necessitates a multi-dimensional approach combining historical, clinical, psychological, and neurophysiological evaluations. These thorough assessments remain fundamental in providing a framework for tailored interventions, ultimately aiming at guiding the adolescent toward recovery within their unique social and psychological context.
Results and Outcomes
The outcomes of treating Complex Regional Pain Syndrome (CRPS) and Functional Neurological Symptom Disorder (FNSD) in adolescents vary considerably based on the individual’s circumstances, the treatment modalities employed, and the involvement of a multidisciplinary care team. Initial assessments following the implementation of comprehensive treatment strategies have shown promising results, highlighting both symptomatic relief and functional recovery in many cases.
Clinical studies indicate that patients undergoing a multi-faceted approach—including physical therapy, cognitive-behavioral therapy (CBT), and appropriate pharmacological interventions—often experience notable improvements in pain management and mobility. One longitudinal study observed that adolescents with CRPS who adhered to a structured physical therapy program demonstrated significant enhancements in their ability to perform daily activities. Specifically, the incorporation of desensitization techniques allowed many participants to gradually decrease their reliance on pain medications while simultaneously restoring function to affected limbs (Johnston et al., 2020).
The psychological component of treatment, particularly CBT, has been shown to lead to substantial changes in the adolescents’ perceptions of pain and disability. By equipping patients with coping strategies, CBT has helped reduce anxiety and depressive symptoms often associated with CRPS and FNSD, thus fostering better engagement in physical rehabilitation. Quantitative analyses have revealed that patients who underwent CBT in parallel with physical rehabilitation reported lower pain scores and improved mental health indices compared to those who received physical therapy alone (Smith et al., 2021).
Interdisciplinary collaboration dramatically enhances treatment effectiveness. Regular communication among healthcare providers ensures that any concerning developments are promptly addressed, and therapeutic strategies are continuously optimized. For instance, an integrated approach involving pain specialists, physiatrists, and psychologists has led to a holistic understanding of the patient’s challenges, thereby streamlining treatment modifications, which are crucial in achieving functional improvements.
From a clinical perspective, outcome measurement tools are vital in assessing progress. The use of standardized questionnaires such as the Visual Analog Scale (VAS) for pain and the Pediatric Quality of Life Inventory provides objective metrics to track changes over time. Patients often report significant increases in overall quality of life post-treatment, underscoring the importance of employing these evaluative tools in clinical practice.
The medicolegal implications of documenting treatment outcomes cannot be underestimated. Specifically, thorough documentation may support disability claims and educational accommodations necessary for affected adolescents. In cases where a patient’s functioning remains substantially impaired despite active treatment, precise records of interventions and their effects become essential in legal proceedings, providing evidence that may inform decisions regarding compensation or school-based support services.
Moreover, relapse rates for adolescents with CRPS and FNSD are compelling factors in evaluating long-term outcomes. While early interventions generally yield positive results, there is an observed subset of patients who may experience recurrent symptoms even after significant initial recovery. Longitudinal tracking of these adolescents highlights the need for ongoing support and potential re-evaluation of treatment plans, which can subserve both clinical needs and medicolegal aspects.
In conclusion, favorable results from contemporary treatment strategies illuminate the potential for recovery in adolescents diagnosed with CRPS and FNSD. The interplay between physical rehabilitation, psychological support, and effective pharmacological management serves as a foundation for positive clinical outcomes. Regular assessment and documentation are integral to optimizing treatment approaches and addressing any emergent challenges, with extensive implications for the patient’s clinical care and any associated legal considerations.
Future Directions
Emerging trends in the management of Complex Regional Pain Syndrome (CRPS) and Functional Neurological Symptom Disorder (FNSD) in adolescents indicate that continued exploration of innovative treatment modalities and assessment methods is vital for enhancing patient outcomes. As our understanding of these complex disorders evolves, the integration of advanced therapeutic techniques and technologies will likely play a crucial role in refining treatment approaches.
One key area for future exploration is the utilization of neurorehabilitation technologies. Virtual reality (VR) and augmented reality (AR) settings have shown promise in not only engaging patients during rehabilitation but also in creating immersive environments that can reduce pain perception through systems of distraction and controlled exposure. Research has demonstrated that VR can enhance motor learning in individuals with CRPS, promoting significant improvements in mobility and function by altering pain processing in the brain (Gonzalez et al., 2022). As these technologies become more accessible and applicable, they could potentially revolutionize the standard rehabilitation protocols by providing tailored experiences for adolescents.
Furthermore, the application of telehealth services is anticipated to markedly increase, particularly in the wake of the COVID-19 pandemic. Teletherapy for psychological support and remote physical therapy sessions could enhance treatment accessibility and compliance, particularly for adolescents in rural or underserved areas. This approach not only allows for continuous patient monitoring and timely interventions but also facilitates regular communication among multidisciplinary teams, which is essential for personalized adjustment of treatment plans. Preliminary data suggests that telehealth can maintain or even improve treatment effectiveness for chronic pain conditions, thus paving the way for innovative service delivery methods (Smith et al., 2023).
Another pivotal area for future research lies in the biological mechanisms underlying CRPS and FNSD, particularly in the adolescent population. Understanding the neurobiological pathways and genetic predispositions could inform targeted therapies that address root causes rather than just symptoms. For instance, biomarkers associated with inflammation or neural plasticity might help identify patients who would benefit most from specific interventions. This knowledge could lead to the development of personalized medicine approaches and more nuanced treatment plans that consider individual variations in disease presentation and response to therapies.
Interdisciplinary education and training for healthcare providers is also expected to expand. With a better understanding of CRPS and FNSD through collaborative learning opportunities, professionals from different fields (e.g., psychology, pediatrics, physical therapy) can unite their expertise to establish comprehensive treatment frameworks that prioritize holistic patient care. Workshops and continued integrated training programs could foster a culture of collaboration and innovation in treatment methodologies.
Additionally, advocacy for increased awareness and understanding of CRPS and FNSD at both educational and policy levels will be essential. Raising awareness among educators, school systems, and healthcare policymakers can lead to improved support systems for affected adolescents, particularly concerning school accommodations and mental health resources. This broader societal approach can ensure that young patients receive comprehensive care that encompasses not only medical treatment but also social and educational support.
Finally, the medicolegal landscape concerning CRPS and FNSD will continue to evolve, necessitating vigilant documentation of clinical assessments and treatment outcomes. Healthcare providers should maintain thorough records to ensure that any future legal considerations, such as disability claims or educational modifications, are substantiated with clear evidence of the patient’s condition and treatment history. Engaging legal experts in discussions related to chronic pain in adolescents could yield more robust frameworks to protect patient rights and secure necessary supports.
Overall, the future of treating CRPS and FNSD in adolescents holds great promise through innovative technologies, personalized medicine, and a collaborative, multifaceted approach to care. Continued research, interdisciplinary training, and advocacy will be pivotal in refining treatment pathways and enhancing the lives of young patients struggling with these challenging conditions.