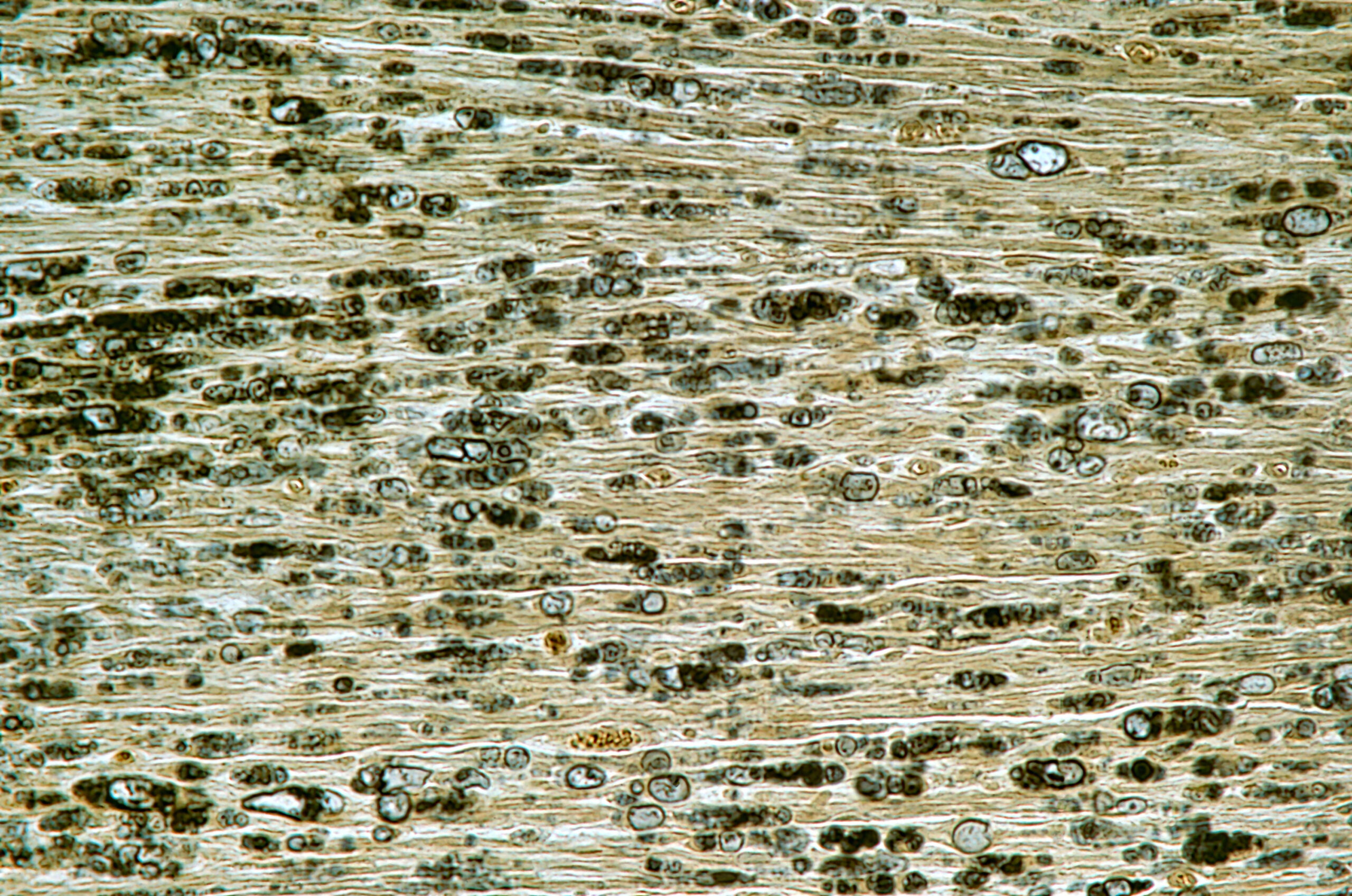
Astrocytes, traditionally viewed as mere support cells, play a pivotal role in the development of post-traumatic epileptogenesis (PTE). They are involved in maintaining ionic homeostasis, the integrity of the blood-brain barrier, neurotransmitter metabolism, and neuronal energy supply. Furthermore, astrocytes are instrumental in modulating neuronal activity, including the exchange of neuronal pyruvate for astrocytic lactate, which enhances neuronal metabolism. They also participate in synaptic information processing by modulating neurotransmitter uptake and release. The activation of astrocytes, a key component of the neuroinflammatory response to traumatic brain injury (TBI), contributes significantly to the pathophysiology of PTE. Astrocytes respond to axonal degeneration, neuronal cell death, and the release of inflammatory factors, which can alter their physiological functioning and impact epileptogenesis. Studies have shown functional changes in astrocytes in epileptic conditions, such as reduced potassium currents and altered gap junction coupling, which are key factors in the development of epilepsy.