Functional Neurological Disorder (FND) is a condition that has long puzzled neurologists, bridging the divide between mind and body. With symptoms that resemble traditional neurological diseases—such as seizures, paralysis, sensory disturbances, or abnormal movements—but without an identifiable structural cause on routine brain imaging, FND is often misunderstood or dismissed. However, recent advances in neuroimaging are providing compelling evidence that changes in brain structure do occur in FND, offering new hope for understanding, diagnosing, and ultimately treating this complex condition.
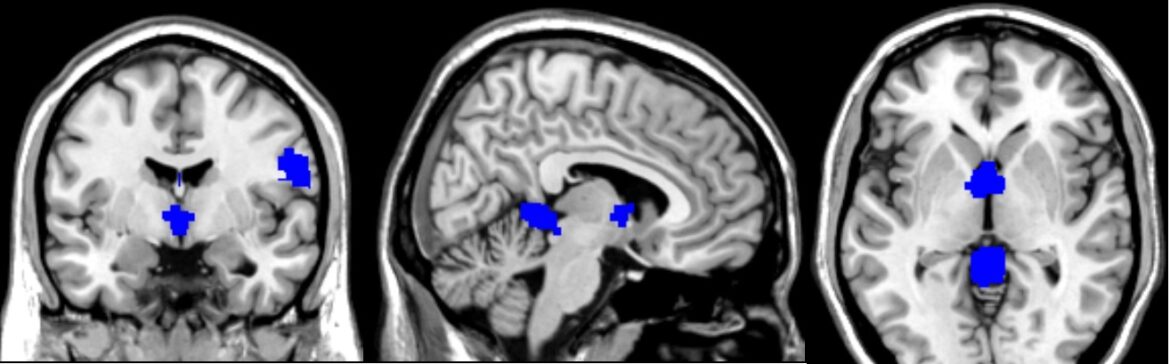
Recent research has brought significant insights into the neurobiological underpinnings of FND by using a technique called voxel-based morphometry (VBM). This method allows scientists to detect subtle differences in brain structure, particularly in grey matter volume, across groups of patients compared to healthy controls. By aggregating data across multiple studies, researchers have conducted a comprehensive voxel-wise meta-analysis that sheds light on where and how the brains of individuals with FND may structurally differ from those without the disorder.
What Is FND?
FND refers to neurological symptoms that cannot be explained by organic disease but are nonetheless real and disabling. The condition affects approximately 6% of patients seen in neurology clinics, making it one of the most common diagnoses in these settings. People with FND may experience motor symptoms like tremors, weakness, or gait abnormalities, or sensory symptoms such as numbness and pain. Others may have non-epileptic seizures or problems with speech or vision. FND is more prevalent in women, particularly in mid-life, but it affects all genders and ages.
Diagnosis can be challenging because the symptoms mimic those of other neurological conditions. Historically, diagnosis was one of exclusion, meaning clinicians had to rule out every possible other cause. More recently, the emphasis has shifted to positive diagnostic signs—specific clinical features that are characteristic of FND—making diagnosis more reliable and less stigmatizing.
Moving Beyond Symptoms: Looking Inside the Brain
Until recently, FND was considered a “functional” disorder largely because standard brain scans showed no structural abnormalities. But neuroimaging techniques like VBM are challenging this view. These high-resolution methods can detect small changes in brain anatomy, such as increased or decreased grey matter volume in specific brain regions.
Grey matter is a key component of the central nervous system, consisting mainly of neuronal cell bodies. Its volume in various brain regions is associated with different aspects of sensory processing, motor control, emotion regulation, and cognition. Therefore, changes in grey matter volume may reflect how the brain is adapting—or failing to adapt—in people with FND.
Key Findings: Where the Brain Changes
By analyzing data from studies involving more than 150 patients with FND and nearly 240 healthy controls, researchers were able to map consistent patterns of grey matter changes in the brain. These patterns varied depending on the subtype of FND but showed significant overlap in certain brain regions.
Increases in Grey Matter Volume
Some brain areas showed an increase in grey matter volume in individuals with FND, suggesting possible adaptive changes, heightened activity, or even compensatory mechanisms:
- Cerebellar Vermis (Lobules IV and V): These midline cerebellar structures are known for coordinating motor functions and processing emotional responses. Increases here were particularly prominent in patients with movement disorders.
- Right Postcentral Gyrus: This region corresponds to the primary somatosensory cortex, responsible for processing tactile information. Changes here may reflect heightened attention to bodily sensations or altered sensory processing.
- Left Supplementary Motor Area (SMA): Involved in planning and initiating movement, as well as integrating sensory and emotional cues. This area was consistently found to have increased grey matter in patients with sensory symptoms.
- Thalamus: A central hub for sensory and pain signals, the thalamus also showed increased volume, especially in patients experiencing chronic pain.
Decreases in Grey Matter Volume
Other regions exhibited reductions in grey matter, which might signify loss of function, maladaptive neuroplasticity, or stress-related atrophy:
- Right Inferior Longitudinal Fasciculus: A white matter tract involved in connecting visual processing areas with the limbic system, important for integrating emotional and sensory experiences.
- Left Insula: A critical area for emotional awareness, interoception (the sense of the internal state of the body), and pain perception. Reduction in volume here was observed in patients with sensory symptoms.
- Cingulate Cortex: Specifically, the median cingulate/paracingulate gyri showed decreased volume in patients with functional movement disorders. These areas are involved in emotion, attention, and conflict monitoring.
Interestingly, the structural changes did not consistently correlate with symptom severity or disease duration. This finding suggests that these alterations might be present regardless of how long someone has had symptoms or how severe they are, and could potentially serve as biomarkers for the condition.
Subtypes of FND: Different Patterns of Change
When researchers looked at different subtypes of FND—such as functional movement disorders, sensory-predominant symptoms, and chronic pain—they found distinct patterns of grey matter changes.
- Functional Movement Disorders: Increased grey matter in the cerebellar vermis and decreased volume in the cingulate cortex were observed. This points to dysfunction in motor coordination and emotional regulation pathways.
- Sensory-Predominant FND: These patients had increased grey matter in the supplementary motor area but decreased volume in the insula, suggesting a disconnect between bodily sensations and emotional processing.
- Chronic Pain FND: Patients with chronic pain showed increased grey matter in the thalamus, frontal gyri, and cerebellum—regions associated with pain processing, emotional modulation, and executive function. No significant areas of decreased grey matter were found in this group, raising the possibility that chronic pain may be linked to a state of heightened sensitivity or vigilance in the brain.
What Do These Changes Mean?
The brain regions implicated in FND—particularly the insula, cingulate cortex, thalamus, and cerebellum—are heavily involved in integrating sensory, motor, emotional, and cognitive information. Disruptions in these circuits could explain many of the symptoms seen in FND. For example:
- The Insula: Often called the “hub of awareness,” the insula integrates sensory input with emotional context. Dysfunction here could lead to a distorted perception of bodily sensations.
- The Thalamus: As the gateway for sensory information, changes here could impact how pain or movement signals are processed and perceived.
- The Supplementary Motor Area: Overactivity or structural changes in this region might contribute to involuntary movements or altered motor control.
- The Cingulate Cortex: This area plays a key role in monitoring conflict and managing emotional responses. Its involvement may relate to difficulties in regulating distress and attention in FND.
Neuroplasticity and the Emotional Brain
One striking aspect of the findings is the overlap between brain regions affected in FND and those involved in processing stress, trauma, and emotional memory. For example, childhood trauma has been associated with structural changes in the insula and anterior cingulate cortex—regions that were also implicated in this research.
This raises intriguing questions: Are these brain changes a cause or a consequence of FND? Do they reflect a brain that has adapted to stress in a maladaptive way? Could interventions that target these circuits—such as cognitive-behavioral therapy, physical rehabilitation, or even neuromodulation—help reverse or compensate for these changes?
The Future: Biomarkers and Better Diagnosis
The identification of consistent grey matter changes opens the door to using these structural differences as biomarkers for FND. Biomarkers could help confirm diagnosis, differentiate FND from other neurological conditions, and guide personalized treatment strategies.
However, more research is needed. Longitudinal studies that follow patients over time could determine whether these brain changes are stable, progressive, or reversible. Integrating structural imaging with functional studies and clinical assessments will be crucial to build a more complete picture.
Conclusion: Reframing the Narrative
FND has long occupied a grey area between neurology and psychiatry, often leading to misunderstanding and stigma. But the growing body of neuroimaging evidence—including robust analyses of structural brain changes—is helping to reframe FND as a brain-based disorder with identifiable neurobiological markers.
Understanding that FND involves real, measurable changes in brain anatomy not only validates patients’ experiences but also provides clinicians with new tools for assessment and intervention. As our understanding deepens, we move closer to a future where diagnosis is quicker, treatment is more targeted, and stigma is replaced by empathy and evidence.