Introduction
Trauma leaves a profound mark on the brain, but not all individuals respond to it in the same way. While some develop chronic psychiatric conditions such as post-traumatic stress disorder (PTSD), others demonstrate remarkable resilience. What determines this difference? One key lies in the patterns of brain connectivity and neurobiological function before, during, and after trauma.
The diagram above illustrates the evolving patterns of brain region activity and structural changes across three critical windows: pre-trauma, peri-trauma, and recovery. Each phase represents a unique neurobiological landscape, shaped by the interaction between emotional regulation systems, threat detection networks, and higher cognitive processes.
Let’s take a guided tour through the image and explore how brain connectivity relates to resilience — and what this means for trauma-informed care and recovery interventions.
I. Pre-Trauma Brain Connectivity: Laying the Neurobiological Groundwork for Resilience
Before trauma occurs, the brain’s baseline state plays a crucial role in shaping an individual’s vulnerability or resilience to future stressors. Certain regions, particularly in the prefrontal cortex and limbic system, are responsible for emotional regulation, threat appraisal, and memory consolidation. The diagram highlights several key regions and pathways with either positive (green) or negative (red) associations between their connectivity and resilience.
Key Brain Regions and Findings in the Pre-Trauma State:
- Dorsal Anterior Cingulate Cortex (dACC)
- Marked in purple, the dACC is involved in conflict monitoring and the regulation of autonomic responses to threat.
- Increased reactivity here is negatively associated with resilience — individuals showing hyperactivity in this region may be more prone to maladaptive stress responses.
- Ventromedial Prefrontal Cortex (vmPFC)
- This area is crucial for emotional regulation, safety signaling, and extinction of fear responses.
- When associated with volume, thickness, and reactivity, higher connectivity of the vmPFC correlates positively with resilience.
- Frontal Pole and Locus Coeruleus (LC)
- The frontal pole is involved in higher-order cognition and decision-making.
- The LC, a brainstem nucleus, regulates norepinephrine release and is involved in arousal and alertness.
- In this pre-trauma state, increased reactivity in the LC is negatively associated with resilience, suggesting that a hyperaroused baseline may increase risk for PTSD.
- Amygdala and Hippocampus
- Key nodes of the limbic system, the amygdala governs threat detection, while the hippocampus is involved in contextual memory.
- Excessive reactivity or abnormal volume in these areas prior to trauma exposure is linked with lower resilience.
What This Means:
Resilient individuals often show stronger connectivity and structural integrity in emotion-regulating regions like the vmPFC, while showing lower reactivity in threat-detection circuits such as the dACC and amygdala. Pre-trauma neurobiology thus sets the stage for either adaptive or maladaptive responses to future stress.
II. Peri-Trauma Phase: The Brain in Crisis Mode
The peri-trauma window—when an individual is exposed to trauma—represents a critical turning point. During this time, real-time neural processes influence the encoding of trauma memories, autonomic arousal, and the immediate emotional response. These neurobiological dynamics can either lead toward recovery or push the system toward chronic dysfunction.
Highlighted Brain Areas During Peri-Trauma:
- Dorsolateral Prefrontal Cortex (dlPFC)
- Seen in red with a positive association (green link), this area supports working memory and cognitive control.
- Stronger functional connectivity here may buffer individuals against overwhelming emotional responses.
- Rostral and Dorsomedial ACC (rACC, dmPFC)
- These areas modulate attention and emotion during stressful events.
- Hyperactivity in the rACC is negatively associated with resilience.
- Insula and Middle Temporal Gyrus
- These regions process interoceptive awareness (the perception of internal bodily states) and emotional salience.
- Reactivity in the insula is associated with lower resilience, reflecting its role in heightened threat perception and autonomic arousal.
- Periaqueductal Gray (PAG)
- The PAG is a midbrain region implicated in defensive behaviors and pain modulation.
- Connectivity with the hippocampus and vmPFC during trauma exposure can influence fear response generalization.
- Temporal Pole and Amygdala Complex
- These regions help encode emotionally salient memories.
- Overactivation during trauma correlates with poor outcomes, such as intrusive recollections or dissociation.
- Posterior Cingulate Cortex (PCC)
- Part of the default mode network (DMN), the PCC may play a role in autobiographical memory and internal mentation.
- Interestingly, its functional connectivity with prefrontal areas may be protective when maintained.
Interpretation:
The peri-trauma brain is a battlefield of competing signals — those that amplify fear, and those that work to control it. If regions such as the dlPFC and vmPFC can successfully engage and regulate limbic activity, the individual is more likely to process the trauma adaptively. On the other hand, hyperactivation in the insula, rACC, or amygdala can imprint trauma deeply into memory, paving the way for PTSD.
III. Recovery: The Rewiring of the Brain After Trauma
The recovery phase is where neuroplasticity — the brain’s ability to reorganize — becomes central. This stage offers both danger and opportunity. Individuals who maintain or strengthen connections in emotion-regulating networks are more likely to recover, while those who continue to show dysregulated connectivity may develop persistent symptoms.
Recovery-Phase Neuroanatomy:
- Medial Prefrontal Cortex Complex (dmPFC, dACC, vmPFC)
- Strengthening of connectivity in these areas (especially vmPFC) is linked with improved resilience.
- Notably, vmPFC activation is associated with emotional reappraisal and extinction of fear.
- Orbitofrontal Cortex (OFC)
- Associated with reward processing and decision-making.
- Positive connectivity from the OFC to limbic regions may reflect more adaptive emotional processing.
- Amygdala-Hippocampus Axis
- With time, modulation of this pathway is essential for contextualizing trauma memories and reducing emotional reactivity.
- Thalamus and PAG
- The thalamus serves as a relay for sensory and cognitive inputs, while the PAG continues to influence arousal and defensive responses.
- Regulation here is key to reducing hypervigilance and somatic symptoms.
- PCC and Insula
- Persistent dysregulation in these regions is associated with poor recovery.
- For example, continued hyperactivation of the PCC may underlie rumination or unwanted autobiographical recall.
The Path to Healing:
Neurobiological resilience during recovery is not simply a return to the pre-trauma state. Instead, the brain forges new pathways — strengthening executive control, dampening limbic overdrive, and restoring interoceptive balance. Interventions such as trauma-focused cognitive-behavioral therapy (CBT), mindfulness, or even neuromodulation techniques (like transcranial magnetic stimulation) may help promote these recovery-facilitating connections.
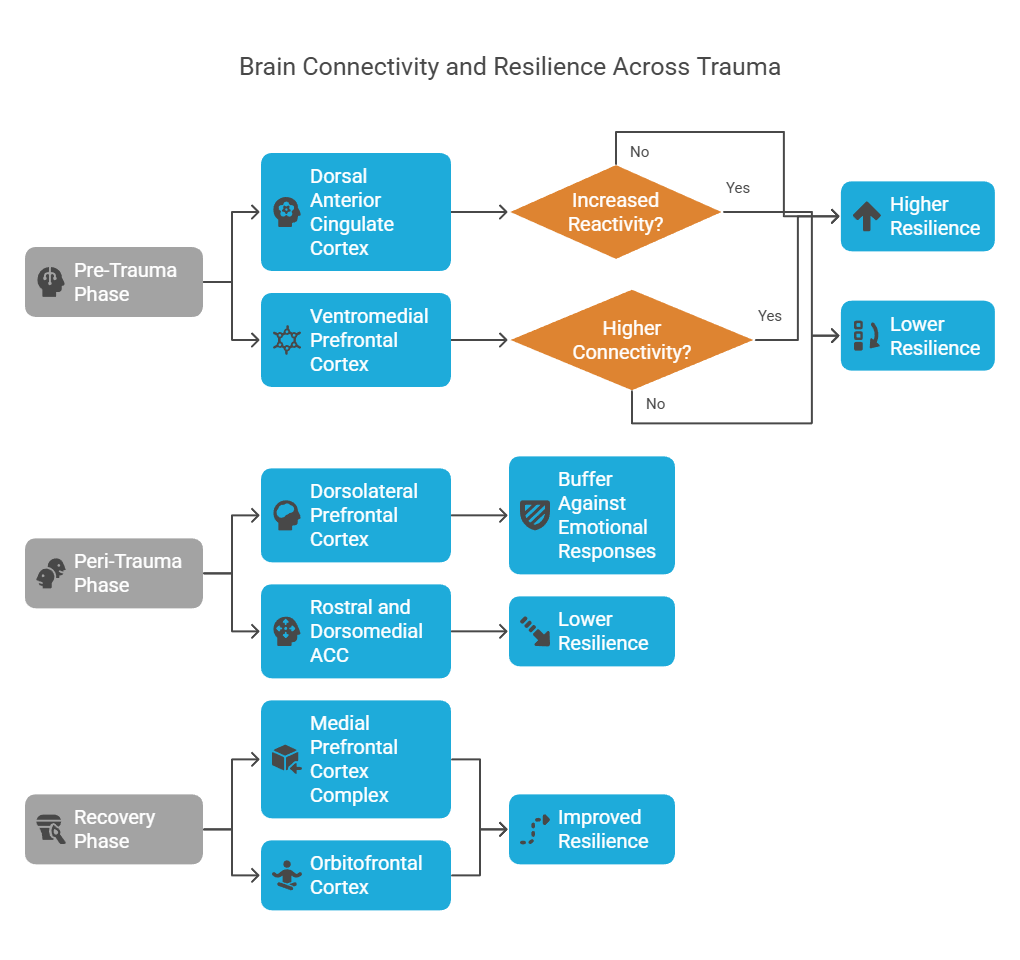
To complement the neuroanatomical map above, the flowchart below provides a simplified visual summary of how different brain regions contribute to resilience or vulnerability across the trauma timeline: pre-trauma, peri-trauma, and recovery.
This schematic breaks down key neural hubs, their role in stress processing, and the outcomes associated with their activity:
Pre-Trauma Phase:
Dorsal Anterior Cingulate Cortex (dACC): Higher reactivity in this region is associated with lower resilience.
Ventromedial Prefrontal Cortex (vmPFC): Higher connectivity in this region supports greater resilience, while reduced connectivity may predispose individuals to maladaptive stress responses.
Peri-Trauma Phase:
Dorsolateral Prefrontal Cortex (dlPFC): Plays a protective role by buffering against emotional dysregulation during trauma.
Rostral and Dorsomedial Anterior Cingulate Cortex (rACC & dmPFC): Overactivation in this region during trauma is linked to lower resilience.
Recovery Phase:
Medial Prefrontal Cortex Complex and Orbitofrontal Cortex (OFC): These regions are central to emotional reappraisal, decision-making, and fear extinction. Strengthened activity and connectivity in these circuits are linked with improved resilience during recovery.
The Bigger Picture: Clinical and Research Implications
This image offers a roadmap for understanding how brain connectivity relates to trauma resilience. It also highlights why trauma is not a uniform experience — its impact depends on a complex, dynamic interaction between pre-existing brain function, acute responses, and recovery mechanisms.
Implications for Research:
- Biomarkers of Vulnerability and Resilience
- Identifying individuals with pre-trauma patterns of hyperreactivity or weak connectivity in emotion-regulating networks could allow for early interventions in high-risk populations (e.g., soldiers, first responders).
- Time-Sensitive Interventions
- Treatments may need to be tailored to the trauma timeline. For example, interventions that dampen insular and amygdala activity might be most effective during the acute trauma window, whereas executive control-enhancing strategies may be better suited for the recovery phase.
- Neuroimaging-Guided Therapy
- Future use of fMRI or EEG-based neurofeedback could help patients train specific networks (e.g., vmPFC or dlPFC) to regulate fear responses more effectively.
Clinical Applications:
- Personalized Treatment Plans
- Understanding a patient’s unique neurobiological profile could lead to more precise psychological and pharmacological interventions.
- Preventive Psychiatry
- For those at high risk of trauma exposure, resilience training (e.g., mindfulness, cognitive control training) might be used preemptively to strengthen key circuits.
- Tracking Recovery
- Functional and structural imaging can help track treatment progress and adapt strategies in real time.
Conclusion
Resilience is not a fixed trait — it is a dynamic property of the brain that can be shaped by experience, intervention, and time. The diagram we’ve explored serves as a powerful visual summary of how different regions and their interactions contribute to survival and recovery after trauma. By mapping the neural correlates of resilience across the trauma timeline, we are not only deepening our scientific understanding but also unlocking new avenues for healing.
Whether you’re a clinician, researcher, or someone who has experienced trauma, this evolving map of the brain offers both insight and hope. The path to resilience may be complex, but it is navigable — and increasingly, it can be supported by neuroscience-informed care.
